A study in the Journal of Developmental and Behavioral Pediatrics
Let’s take a look at what they did and what they found…
What They Did
The data was collected as a part of the Norwegian Mother and Child Cohort Study which follows up with families (using questionnaires) at various points across development. For the current study, data from birth, 6 months, and 18 months was included, which included 55,831 infants (data was collected between 1999 and 2008 so all infants that met that criteria were included). Results controlled for maternal age, birth weight, infant sex, gestation, and parity. Sleep variables were categorical, meaning parents did not provide absolute times but rather general times (which is actually likely a strength given the variability in infant sleep from night to night). For total nightly sleep, the categories were set to ≤ 10 hours, 11-12 hours, 13-14 hours, ≥ 15 hours. For night wakings, the categories were 3 or more times per night, 1-2 times per night, several times a week, or seldom/never. Bedsharing was assessed by asking, “Does your child sleep (at least half the night) in the same bed as their mother/father?” with options being Often, Sometimes, and No and were recorded at 6 months for birth, 2 months, 4 months, and 6 months.
In terms of the analyses, the researchers defined a “sleep problem” as ≤ 12 hours of nighttime sleep or nightly wakings at 18 months of age. This brings us to problem #1 with this research: This definition was given by the researchers only and there was no evidence of “problematic” sleep in terms of later outcomes or parental report on these numbers. In fact, parents disagreed with the researchers as only 2.5% of families reported that they felt their child had a sleep problem (compared to the between 26 and 38% defined by the researchers’ criteria). For example, only 9.4% of families who reported nightly wakings found them to be a “problem”.
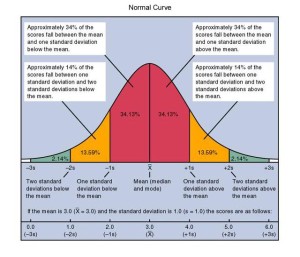
The use of ≤ 12 hours of sleep was because 13-14 hours was the median for the group; however, anyone who is aware of the normal curve (see image) should know that one does not need to fall at the median in order to be classified as “normal”. Indeed, only the smallest of subsets classifies as falling out of the normal range (which is actually in line with the 2.5% of parents reporting sleep problems). The fact that 38.1% of the sample was sleeping ≤ 12 hours while 26.6% had nightly wakings at 18 months suggests this idea of “problem” may be a little overstated, if not downright wrong. If the researchers truly wanted to look at what predicted sleep problems, a better design would have been to look exclusively at the patterns and behaviours of the 1365 children whose parents reported sleep problems instead of the entire sample. However, this was not done, so on we go…
What They Found
With the idea that we’re looking at what predicts nightly wakings and “short” sleep duration, the largest predictor of nightly wakings at 18 months was ≥ 3 wakings per night at 6 months (6.55 times the risk) and the largest predictor of ≤ 10 hours of sleep per 24 hour period (the lowest category, though it was often included with 11-12 hours in other analyses) was ≤ 10 hours of sleep per night at 6 months (14.59 times the risk). This suggests that there is likely a third variable problem going on with something influencing sleep early and later. What that is remains unknown as the study did not look at some of the factors that might lead to this type of waking and sleep duration.
But what of this bedsharing-“sleep problem” association? After all, this is the crux of the study in terms of how the researchers present it and how the media has portrayed it.
The main relationship is that bedsharing at 6 months doubles the risk for nightly wakings and short sleep duration at 18 months. There are a few considerations or explanations for the data on bedsharing that should be mentioned before we caution parents against bedsharing for fear their child will suffer “sleep problems” later as a result.
First, the suggestion that bedsharing at 6 months somehow influences sleep at 18 months without knowing the sleep location of children at 18 months is highly limiting. It is likely that bedsharing at 6 months predicts bedsharing at 18 months and cross-cultural research does show that in societies where infants are bedsharing, the total nighttime sleep is less[2], even if not “problematic”. This is often due to bedsharing infants and children going to bed later (with their parents) and sleeping in some, but not the full amount as societies in which infants sleep alone. In a cross-cultural context, this type of sleep pattern is actually quite normal.
Second, the researchers failed to examine the type of bedsharing that was occurring at the various ages. There is a distinction between reactive and planned bedsharing, both practically speaking but also in infant sleep outcomes. Families who decide to bedshare ahead of time for cultural, personal, or other reasons are considered planned bedsharers whereas families who do not wish to bedshare, but end up bedsharing usually due to early infant “sleep problems” are considered reactive bedsharers. (Note I use quotations when discussing infant sleep problems because often sleep is not the problem, but is a reflection of another problem. However, in our society the focus is on solving the sleep problem instead of looking for the underlying cause.) The distinction is critical when we consider research such as the study presented here.
In line with this idea of reactive bedsharing, there are likely cases where undiagnosed (or diagnosed) health problems influence sleep and the bedsharing relationship. One such example would be reflux in which an infant would likely wake regularly still at 18 months depending on treatment and would have been more likely to bedshare at 6 months due to the need to be close to a parent. Food allergies and sensitivities, which can negatively influence sleep, may lead parents to bring a child to bed for comfort and can persist if undiagnosed, or simply reflect a sensitive system.
The researchers do touch very quickly upon this possibility in saying they did not assess the reasons for bedsharing at 6 months, but suggest it’s not a concern because they controlled for the number of night wakings at 6 months in their analyses. The problem with this explanation is that, from what they have shared, they didn’t account for this type of interaction because of the way regression works. By the looks of things, they used hierarchical methods to adjust for some variables. What the controlling is doing is giving people the effect of bedsharing at 6 months after removing all the variance explained by previous night wakings instead of looking at the interaction between the two. Thus, this remains a question of interest. (For more information and a review of the research on types of bedsharing and outcomes, see [3].)
One additional factor to consider with bedsharing is how often people report it honestly. Two reasons can affect maternal report of bedsharing: (1) There is often such anti-bedsharing messages from health professionals that parents don’t actually admit to it for fear of repercussions or people finding out, and (2) Many people don’t consider themselves “bedsharers” if their child doesn’t start the night in bed, even if said child ends up in bed part way through the night most nights. Unfortunately, this limitation is inherent in almost all research in bedsharing, though the first concern is particularly salient here as people’s information was all linked. The second one was less of a concern given the wording of the question (including half the night in the question) but also requires parents to think about how much half the night is. People who don’t want to be seen as bedsharing will err on the side of saying “no” even if their behaviour fits.
Third, and perhaps most importantly, the role of breastfeeding is very unclear. Although the researchers acknowledge that breastfeeding is a concurrent predictor for night wakings and shorter sleep duration at 6 months, they did not assess breastfeeding at 18 months or the interaction between breastfeeding and bedsharing. They did find that of the children who were predominantly breastfeeding at 6 months (no formula and no solids, but open to “other” liquids), 38.5% were regular bedsharers compared to 12.1% of families who were predominantly using formula, so the failure to consider that the same type of overlapping relationship may exist at 18 months is odd (and breastfeeding was also a predictor of night wakings and shorter nighttime sleep duration). I realize that many 18 month olds are not nursing (indeed only 14.8% of the sample were predominantly breastfeeding at 6 months), but this group may be the one small group in which the high wakings persist across time, and this may not be a bad thing.
What They Suggest and What They Really Can Suggest
The researchers use their data to subtly suggest causation in the bedsharing-night waking relationship and go a step further by suggesting that parents consider the relationship when planning sleeping arrangements. This is highly premature given the findings and unavailability to test the likely confounds that would result in such an association. The researchers themselves acknowledge certain variables are missing that would inform on the current developmental trajectory and associations, specifically daytime sleep (a huge limitation as it is linked to nighttime sleep duration), parent psychopathology, parent sleep problems, and actual night wakings (as opposed to signaled night wakings). I would add to this what I have already mentioned—breastfeeding and bedsharing behaviours at 18 months—as well as the use of a routine, the use of sleep training, parent sleep more generally (as parents need not have a “problem” to influence their child’s sleep genetically or behaviourally), sibling sleep behaviours, and child health (specifically things like reflux and food sensitivities that can influence sleep).
As is, what this research provides is another way to look at infant sleep trajectories. In this vein, the researchers are much more realistic in what the data provides and even suggest that what they show is that both night waking (at 6 months and 18 months) and bedsharing in infancy should be considered developmentally or culturally normative. Sadly this is lost in the use of language that suggests these normative behaviours are “problematic” when there is no evidence to support this type of diagnostic criteria.
_____________________________________
[1]Hysing M, Harvey AG, Torgerson L, Ystrom E, Reichborn-Kjennerud T, Sivertsen B. Trajectories and predictors of nocturnal awakenings and sleep duration in infants. Journal of Developmental and Behavioral Pediatrics 2014; 35: 309-16. [2]Mindell JA, Sadeh A, Wiegand B, et al. Cross-cultural differences in infant and toddler sleep. Sleep Medicine 2010; 11: 274-80. [3]Cassels TG. ADHD, sleep problems, and bed sharing: future considerations. The American Journal of Family Therapy 2013; 41: 13-25.







Thank you! It’s so good to see someone doing a logical and calm assessment of research.