 The question of inductions can be a heated one at times, with proponents of natural birth shunning the idea of artificially inducing something that should happen naturally. We hear comments like, “The baby knows when to come out” and therefore we are wrong to intervene. But this ignores that women have tried many methods over the years to bring on labour – from red raspberry leaf tea, to lots of sex, to exercises, to eating spicy food, and so on and so forth. So the idea of “induction” isn’t really new, but our methods have changed considerably, moving from old wives’ tales (some of which do seem to work to at least ripen the cervix) to more medicalized procedures.
The question of inductions can be a heated one at times, with proponents of natural birth shunning the idea of artificially inducing something that should happen naturally. We hear comments like, “The baby knows when to come out” and therefore we are wrong to intervene. But this ignores that women have tried many methods over the years to bring on labour – from red raspberry leaf tea, to lots of sex, to exercises, to eating spicy food, and so on and so forth. So the idea of “induction” isn’t really new, but our methods have changed considerably, moving from old wives’ tales (some of which do seem to work to at least ripen the cervix) to more medicalized procedures.
Notably, I don’t think anyone in their right mind is suggesting we don’t induce when there’s a medical necessity (at least I personally hope not) as inductions for certain medical conditions, like preeclampsia or HELLP, can save lives. The question is really about the safety and use of a medical procedure when it’s not medically indicated.
Here I will cover what the research has shown to date on the safety of elective inductions separated by gestational age…
Pre-Term (< 37 weeks)
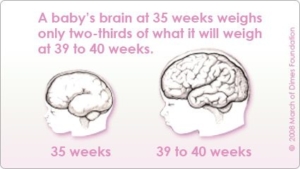
If you’ve managed to get an elective induction prior to 37 weeks, you should probably sue your doctor because we know that prior to that time, the risks for neonatal complications are high even when women are induced for medical reasons (or have to have a c-section) or simply go into spontaneous labour at that point, like a 3-7 times increased risk for neonatal morbidity and mortality Term (37-41 weeks) Although many consider term to run to 42 weeks, in the literature it is often set at 41, meaning I will use that here because it’s how the research is divided. Within term, there seems to be two separations, 37-39 weeks and then 39-41 weeks. With respect to elective inductions up to 39 weeks, in a representative cohort sample observational study (meaning they looked at actual inductions instead of planned), 17.2% of elective inductions at 37 weeks ended up in the NICU versus 7% at 38 weeks and 6% at 39+ weeks[4]. Notably, numbers at 37 and 38 weeks were significantly greater than those at 39 weeks. Additionally, the likelihood of ending up with a c-section was around 13% for all three gestational age groups, but was influenced by the degree of dilation with induction and parity. For example, nulliparous pregnancies at 0 cm dilated at time of induction had a 50% risk of c-section and this number decreased to 10% if 5 cm dilated. The numbers were smaller for multiparous pregnancies with numbers ranging from 15% (0 cm) to 0% (5 cm). But what of 39-41 weeks? Well, another retrospective cohort study focusing only on nulliparous women (who, based on the previous research clearly have greater risk of negative outcomes) between 39 and 41 weeks gestation found no significant differences for women with a favourable cervix at induction[5]. The only difference was the amount of time between admission and delivery, with the electively induced group having a significantly longer stay. However, another study from Belgium looking at nulliparous pregnancies with gestational age of 38 to 41 weeks found increased risks of c-sections, instrumental delivery, epidurals, and NICU transfers[6]. Seeing as both studies compare induction to “expected management of pregnancy”, this could raise questions about what this expected management actually is. Little is said, but it is possible that the higher rates of medical interventions in all births in the US mask some of the effects of induction that are showing up in other countries where these interventions are less common. Notably a review of the research on induction looking at 39, 40, and 41+ weeks found such a paucity of research at 39 and 40 weeks that they couldn’t make any conclusions[7]. Therefore, these mixed results must be taken as just that – mixed results. Post-Term (41+ weeks) I hate having to write that post-term is 41+ weeks, but this is the research definition and therefore I must utilize it to make any sense of the research. Cochrane has done a review on the policy of induction versus expected management at term or post-term, with results relevant to 41+ weeks[8]. There were a total of 22 studies over 9383 women included (only 5 studies were USA so truly global). They found that a policy of induction resulted in a 69% decreased risk of perinatal death when mom was induced after the 41 week point. Meconium aspiration was also reduced 50% in the induction group and there were no differences in NICU admissions. There was a nearly significant 86% increase in birth asphyxia for the induction group and operative vaginal births were increased 10%. These results speak pretty clearly in favour of a policy of induction; however, there are a couple factors to consider. First, by the authors own examination only 3 studies were rated as having a low-bias, meaning the remaining 19 trials were at risk of high-bias and may influence the overall results. Second, the review included randomized trials and they were randomized by policy not by actual outcome. This means that there were probably some women in the induction group who were expectantly managed and some women in the expectantly managed group who were induced. The authors are clear to state that these results speak only to what policy a caregiver can have, not what might actually occur. Before we throw the review out completely, there is another review[7] which examined randomized controlled trials (RCTs; like the Cochrane review) and actual outcomes in this same range. The RCTs found that being in the expected management group over 41 weeks gestation was associated with a 21% increase in c-sections and a 104% increase in meconium stained fluid compared to being in the induced group; however, the actual outcome (observational) studies found a 27% decrease in c-sections for those who experienced expected management versus induction, but the authors argue there was no control for gestational age meaning these may be biased in some way towards the expected management group (though this assumes that the expected management group is of lower gestational age and I honest-to-goodness don’t know that that is the case). What is interesting is the finding that the observational studies are not matching the RCTs. This suggests that policy and practice are actually two very different things and we have to be cognizant of this when interpreting the data. Having a policy of induction does not mean every mother chooses to induce. The studies also do not provide additional analyses by gestational age over 41 weeks. As mentioned several times, it is not uncommon to consider 42 weeks still “term” and thus expected management between 41 and 42 weeks may account for the findings of the observational studies. Further, other providers may simply wait until 42 weeks to induce. ***** Overall, induction when not medically warranted is something we may want to be careful of. Though RCTs suggest benefits of inductions post-term, this has not played out in the few observational studies there are. Research definitely needs to examine what factors might be influencing this mismatch in the research. One further possibility is that the policy of induction includes maternal choice and information by caregivers whereas a policy of expected management is too far against induction or not checking regularly to note early problems; this could mean that cases where there may be the beginnings of problems are not being induced as they should be. That may not be it at all, I just speculate, but by speculating, I hope to point out that there are myriad reasons why the research is not nearly as clear as one would hope. What to do? Well, at term or pre-term, it seems there is very little reason to electively induce, and more likely some downfalls to that decision. Although post-term the risks seem to be slightly different though it’s difficult to reach a conclusion. It seems fair, however, to say that being open to an induction post-term may be beneficial, and that monitoring the situation is important. [Image Credit: Babybelly Australia]
[1] Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, et al. Effect of late pre-term birth and maternal medical conditions on newborn morbidity risk. Pediatrics 2008; 121: e223. [2] Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR. Differences in mortality between late pre-term and term singleton infants in the United States, 1995-2002. J Pediatr 2007; 151: 450-6. [3] Talge NM, Holzman C, Wang J, et al. Late-preterm birth and its association with cognitive and socioemotional outcomes at 6 years of age. Pediatrics 2010; 126: 1124-31. [4] Clark SL, Miller DD, Belfort MA, et al. Neonatal and maternal outcomes associated with elective term delivery. American Journal of Obstetrics & Gynecology 2009; 200: 156.e1-156.e4. [5] Osmundson S, Ou-Yang RJ, Grobman WA. Elective induction compared with elective management in nulliparous women with an unfavourable cervix. Obstetrics & Gynecology 2011; 117: 583-7. [6] Cammu H, Martens G, Ruyssink G, Amy JJ. Outcome after elective labor induction in nulliparous women: a matched cohort study. American Journal of Obstetrics & Gynecology 2002; 186: 240-4. [7] Caughey AB, Sundaram V, Kaimal AJ, Cheng YW, Gienger A, Little SE, Lee JF, Wong L, Shaffer BL, Tran SH, Padula A, McDonald KM, Long EF, Owens DK, Bravata DM. Maternal and Neonatal Outcomes of Elective Induction of Labor. Evidence Report/Technology Assessment No. 176. (Prepared by the Stanford University-UCSF Evidenced-based Practice Center under contract No. 290-02-0017.) AHRQ Publication No. 09-E005. Rockville, MD.: Agency for Healthcare Research and Quality. March 2009. [8] Gulmezoglu AM, Crowther CA, Middleton P, Heatley E. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev 2012; 6: CD004945.




This was a great article but I was surprised you didn’t touch on the risk of placental insufficiency post term and the risk of stillbirth as a primary indication for induction of labour.