Disclaimer: The following article involves topics of a medical nature. This commentary is not supposed to take the place of advice given by a medical professional (midwife or doctor). It simply provides research information regarding the use of certain drugs and can only be considered general information, not specific advice for a given person.
 Epidural. That one little word has the power to start wars. Well, not literally, but if you get women in a room together and get them to start talking about the issue of drugs during delivery, you’re bound to end up with your own small scale war. On the one hand, there are those who feel that epidurals are bad and shouldn’t be given to laboring women at all, on the other there are those who feel that it’s nobody else’s business what they do during their delivery and that if they want pain medication, no one should judge them for it. Then there’s a third hand which is where I stand. My view in a nutshell: The development of the epidural was a great scientific discovery that has the power to help women who NEED it in labor. It has its place in the world of childbearing, but it has also been VASTLY overused and many of those who opt for it have no idea what it is that they’re choosing to do. Most women are unaware of the risks associated with the epidural and though some would opt for it with that information, some might not and it is our duty to ensure women are aware of risks they are undertaking.
Epidural. That one little word has the power to start wars. Well, not literally, but if you get women in a room together and get them to start talking about the issue of drugs during delivery, you’re bound to end up with your own small scale war. On the one hand, there are those who feel that epidurals are bad and shouldn’t be given to laboring women at all, on the other there are those who feel that it’s nobody else’s business what they do during their delivery and that if they want pain medication, no one should judge them for it. Then there’s a third hand which is where I stand. My view in a nutshell: The development of the epidural was a great scientific discovery that has the power to help women who NEED it in labor. It has its place in the world of childbearing, but it has also been VASTLY overused and many of those who opt for it have no idea what it is that they’re choosing to do. Most women are unaware of the risks associated with the epidural and though some would opt for it with that information, some might not and it is our duty to ensure women are aware of risks they are undertaking.
The biggest hurdle to overcome when trying to get people to educate themselves about drugs and childbirth is debunking the myth that whether or not one uses pain medication should be no one’s business but their own. The main argument is that their decision doesn’t affect anyone else so why should the rest of us care? Unfortunately for them, there is a couple of glaring fallacies to this argument. First and foremost, it does affect someone else – your baby. It continues to amaze me how some women consistently forget that there’s this tiny human who is completely dependent upon us to consider its needs (or even those that realized it throughout pregnancy seem to forget it during the birthing process); and because they forget, the needs of this tiny human are often ignored. Second, even if it did only affect you, if it can hurt you, then we as a society have the moral obligation to make you aware of it so you can make an informed decision.
But what could be so wrong with epidurals? I mean, they make giving birth painless and easy, right? Yes and no. While an epidural may take away the pain for mom, it can (and regularly does) make labor more difficult resulting in more interventions than a drug-free birth. There is ample evidence that women who receive an epidural are much more likely to require the use of oxytocin/pitocin
There seem to be a couple contributing factors to this cascading effect of interventions:
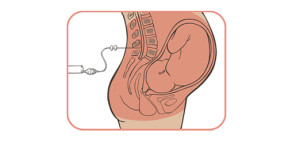
The first factor is that once you get an epidural, you’re bed-bound. No moving, walking, etc. for fear that you screw up that spinal and really hurt yourself. And as any midwife will tell you, movement is key to getting baby out – gravity is your best friend during delivery. So when you force a woman to stop moving, you slow things down labor-wise. Second, epidurals (given when not needed ) weaken your contractions and, as I’m sure you’re aware, you need contractions to continue or, once again, you end up with even bigger problems. So if labor slows for either of these reasons, you need to make it faster, which is why you add in the oxytocin/pitocin (though I’ve heard of doctors starting with the pitocin just to speed things up—heaven forbid they miss a golf game—and the intense contractions require the epidural to slow it down again and kill the pain). Of course, the use of pitocin then results in even stronger contractions which can be too much for baby, meaning you end up with baby in distress and the need for an emergency c-section. Or if the pitocin doesn’t speed things up enough, you could end up with the emergency c-section for failure to progress. These three interventions are much more intertwined than many people realize.
Perhaps, though, you’re lucky enough to just have the epidural and avoid the pitocin or c-section. That means you’re in the clear, right? Wrong. You also get to worry about infection. The use of epidurals is also linked with moms getting an intrapartum fever and therefore needing antibiotics during delivery. The use of antibiotics during delivery is linked to higher rates of sepsis in newborns, requiring antibiotic treatment at birth[6]. Intrapartum fever has also been related to various other adverse effects in newborns, including seizures[7]. So even if you manage to avoid other maternal interventions, you run the risk of causing more harm to your newborn.
Still think the epidural is all fun and games? Hopefully not, but there’s one more thing to consider: The reason most women get an epidural is to kill the pain; however, have you actually thought about why there’s pain during childbirth? If there were no reason for pain in childbirth, there wouldn’t be any, so obviously it’s there for a reason. And while we may never know the exact reason (after all we can’t exactly ask evolution), we can hypothesize based on neonatal outcomes. One of those reasons is hypothesized to be a way to make sure mom stops what she’s doing and goes someplace safe. But really, there could be a way to do that without pain per se so it’s questionable how helpful the pain is for that aspect of birth. Another hypothesis, and one really worth thinking about, is that the pain is there to produce endorphins to help the baby through labor as well. It is believed that babies can’t produce their own endorphins and so require mom’s endorphins to help with the pain (in case you hadn’t considered it, babies draw an even shorter straw than mom does during this whole labor thing), and the use of an epidural, while killing pain for mom, means baby gets no pain relief during labor[8][9]. That is also one possible reason why babies may go into greater distress, leading to the necessity of an emergency c-section, even without that intermediary, pitocin[5].
I did say, though, that epidurals were useful at times and it’s worth reminding people why they were developed. For starters, they’re fantastic for women who have to have a c-section because it allows them to be awake and meet their baby much sooner than if they had to be given a general anesthetic. If you ask any mother who’s had a c-section, they can feel much better about it because they get to meet baby so soon thereafter. For the non-c-sectioners out there, epidurals are there primarily to help with very long or very painful labors (though the two usually go hand-in-hand), as a labor that goes for too long typically involves mom being too tense to relax at all, meaning there’s no room for baby to get in the proper position to come down. This can lead to distress for baby, who’s trying to get out, and can be incredibly dangerous, risking both mom and baby’s life (which is why the notion that drugs are never good is just as asinine as that that they are harmless). Women with back labor are particularly prone to extended and hugely painful labors, and can result in women being in labor for days (sometimes up to five days), and if you’d been in labor that long (with each contraction making you feel like someone’s breaking your back because of the back labor), you might need something to help things along as well. The epidural relaxes mom enough to allow her to “open up” and let the baby down into the birthing canal and continue with a safe labor. Notably, in these cases the epidural doesn’t actually slow labor – it speeds it up. That is one sign that something is doing the job it’s supposed to—it helps the process along instead of slowing it. (We only consider cancer treatments effective because they slow down the spread the cancer; if they sped it up, no one would take them, so why is birth any different?)
It’s time to make sure women are informed about the interventions in birth. So that women can take more responsibility for their birthing process, to make sure they know what they’re doing and what’s happening to them at each stage. It’s also time to start thinking of mom and baby as a unit again. Throughout history, mom and baby have been seen as one—co-dependent and in sync—yet in Western cultures we’ve lost this sense of connectedness. Perhaps that’s why it’s so easy for doctors and mothers alike to avoid thinking about the side effects of many interventions. Not everyone will have or even opt for a drug-free labour, but women should at least be given the knowledge of what is happening and what risks are associated with it so they can make informed decisions. [Note: Some have suggested the research is out of date. However, new research supports exactly what was written herein. For more recent studies, please see the following:
Anim-Somuah, M., Smyth, R.M.D., Howell, C.J., 2005. Epidural versus non-epidural or no analgesia in labor. Cochrane Database Syst Rev Issue 4, Art No.: CD000332.
Eriksen LM, Nohr EA, Kjaergaard H. Mode of delivery after epidural analgesia in a cohort of low-risk nulliparas. Birth 2011; 38:317-26.
Greenwell, E.A., Wyshak, G., Ringer, S.A., Johnson, L.C., Rivkin, M.J., Lieberman, E., 2012. Intrapartum temperature elevation, epidural use, and adverse outcome in term infants. Pediatrics 129, e447-e545.
Jonas, W., Johansson, L.M., Nissen, E., Ejdebäck, M., Ransjö-Arvidson, A.B., Uvnäs-Moberg, K., 2009. Effects of intrapartum oxytocin administration and epidural analgesia on the concentration of plasma oxytocin and prolactin, in response to suckling during the second day postpartum. Breastfeed Med 4, 71-82. ]





i posted your blog on my sight and i agree that making women more aware of what happens with an epidural is important but the beginning of you blog there seems to be a lot of judgment on women who chose to get the epidural saying even that it should be regulated. Being someone who is very much pro choice as well as a big birth activist i think it’s important both to educate about dangers but also trust women to make the best choice. no one person can predict a nothers ability to manage pain or experience with pain. refusing women who need the epidural because we think that they should be able to handle it could lead to PTSD for many women as well as lead to increase in PPD both of which can impact the baby as well. women need to know more about the effects of epidurals they also need to be trusted to make the best choice for themselves as well as their babies.
I think you misunderstood the beginning. I was saying that the regulation view is one that is out there, but that my personal belief is that it should be there for women who need it. How we define need is paramount – women who have much difficulty with pain will “need” an epidural and that will manifest itself throughout the labour. Understanding and being able to read a labouring woman’s signs is what trained midwives (and some doctors) are able to do. While this may involve limitations on it, I do believe those limitations would still need to include the trained decision of the professional involved who can take her/his particular client’s needs into consideration.
There is nothing in this article that I disagree with. Well written with common sense. Thankyou
This article is ridiculous! It blows the risks of an epidural extremely out of proportion with the reality. In a hospital setting the risks of recieveing an epidural are greatly reduced as well as any risk of infection. And all risks are very clearly covered in any labor and delivery class. If the epidural is properly administered you can still feel, it just lessens the pain, for a c-section the dose is increased so that the mother will no longer be able to feel. The baby also is going through a lot getting shoved awkwardly through a small hole, that can’t be comfortable for the baby, if anything does go to the baby its probably only enough to help the baby relax. And if taking the drug harmed the baby then OBGYN’s wouldn’t want patients to take it and would strongly advise against it. And just because a baby is groggy does not mean that it’s because of the drug, that baby just went through a tramatic and tiring experience it is completely natural for the baby to be tired. And I have known many mothers who gave birth naturally to then have a very groggy baby, and I’ve known many mothers, myself included, who used some sort of pain relief and gave birth to very alert babies. It is entirely the mother’s choice and writing a very biased article is not going to change that.
Anissa: I’m sorry you feel this way, but all the risks I spoke of come from scientific research trials and were simply stated as they have been found to occur. I’m not sure where you’re from, but I know many people who have been to prenatal classes and had none of the risks of epidurals covered in their class. Sadly in North America that doesn’t seem to be the norm. As for the reduction of risk of infection in a hospital, that’s simply not true – the infections talked about in the research I cite come about in hospitals, not at home or anywhere else. (It’s one of the reasons why home birth has been found to be safer in many categories (for low-risk pregnancies) than hospital births.)
I also want to address this idea that OBGYNs wouldn’t want patients to take it if it harmed them or their babies. I strongly suggest you read up on the history of what OBGYNs have offered women in the past and how they have managed to provide drugs and procedures to pregnant women that have had disastrous effects. Thalidomide being the most well-known case. It was a sedative that was given to women for morning sickness without research into how it might affect babies because doctors simply assumed that drugs couldn’t pass to babies in utero. Well, thousands of babies were born without limbs and a high percentage of them died as well. The fact remains that sadly doctors believe they know best and rarely do the testing necessary before administering new drugs or procedures (see how little has been done with vaccines – it’s how we ended up with mercury in them for so long and now questions are raised over aluminum). While I do believe no one intentionally goes out to hurt babies or their moms, whether it be ego or sheer ignorance, too often they do.
I had a baby about 3 months ago. I really wanted to avoid an epidural but after 20 hours of strong contractions every 2 or 3 minutes, I broke down and asked for one. Not long after, my baby was in distress and her heart rate was dropping so I had to have an emergency c-section. I had a long and painful recovery with several complications including infection. We also had a hard time with breastfeeding at first. Both baby and I are doing well now and breastfeeding well too.
Of course I can’t be sure that the epidural caused her distress and ultimately the c-section, but I have wondered about it. In future, I will avoid an epidural and would encourage women to let it be their last resort.
Anissa: I have had 3 children. My first I was completely numb from the waist down and did not feel a thing. I could not feel her move kick, no contractions, nothing. With #2 I was numb for the most part, The only thing I could feel was pressure when it was time to push. #3 was going to be my all natural baby. (I had pitocin and epidural with #1 and 2) I wanted a water birth, no drugs. I had placenta previa. I was so stressed out when I went in (my placenta was still marginally covering) and was to have a c-section (that was not technically needed) that they had me pumped full of all kinds of meds. I think the total was 5 or 6. Again, I was completely numb. The epidural was done correctly. I did not need it any of the times. I thought I wouldn’t be able to handle the pain. I know if I was to have another baby, it will be at home. Drug free. 1st labor lasted from 5:30am-10:22pm(I was induced). 2nd Probably midnite (went into labor natural, pit to speed it up) until about 6pm (same day). With #3 I don’t remember much of anything. I look at the pictures from the OR and I don’t remember a thing. I will NOT have these experiences again.
By the way, thank you for this article. I’m sharing on facebook
Thank you for sharing your story Lindsay! I find it very sad how many women have the same experiences as you and truly regret their birth events. It’s supposed to be a wonderful thing to welcome a child into this world. No one said it should be pain-free though. I hope if you do go for #4 that you get the birth you want!!!
Quote: “It continues to amaze me how women consistently forget that there’s this tiny human who is completely dependent upon us to consider its needs; and because they forget, the needs of this tiny human are often ignored.”
…Unbelievable judgement on your part. It’s usually those people who are the most “sure” of their opinions that are the most disconnected to the reality of others, and in this case, other women. Most women make themselves sick for 9 months worrying about every little twinge, about everything they put in their bodies, about which side of their body to sleep on, whether their bath water is too warm, about whether medication that keeps them healthy will harm the baby, about whether they will be good moms…and you think these women simply forget and ignore the needs of the life inside them at the moment of truth? With all due respect, how dare you?!
I had an epidural at 4cm, and gave birth to my healthy son 9 hours later with the help of my midwife. I pushed for one hour, and though I couldn’t feel a thing, my body was still capable. I did not tear, and I was relaxed, and alert. My baby and I bonded immediately, and I was home with him the next day. For every “horror story,” there are 10 success stories, and you will find as many horror stories among women who went “natural.”
I’m afraid I have to disagree. As a practitioner I observe that it’s more likely to be one success story for every 10 ‘horror’ stories when it comes to the epidural. And with women who go natural ‘in a natural habitat for birth’ primarily home or failing that, a birth centre, for every 1 horror story there will be 10 success stories. Gather with a group of women who have recently birthed and see how many have an epidural story that ends up with them perky, alert, mobile, bonded, breastfeeding well and recovering quickly. Your more likely to hear about pitocin (the tragic side effects of which are only now coming to the fore), the fetal distress, the resus, the caesarean , the infection and then down the line the severe perineal trauma, the backpain and the incontinence. Yes mothers do consider their babies but they need to give consideration too to the way their child is born, the potential for bonding and how they are nourished because these factors have lasting impact on the person. So when considering the needs of their newborn it really ought to include some of the factors listed in the article like increased risk of infection and exposure to antibiotics, increased risk of ‘extracted’ birth with the associated trauma to neck and shoulders, increased risk of a fetal monitor being screwed into their scalp – and yes of course that hurts, why wouldn’t it – increased risk of being severed from their blood supply for ‘resus’, the likelihood that they are forced through a pitocin fueled birth without endorphin pain relief, the likelihood that because of the pitocin that tends to go hand in hand with an epidural, the baby will be starved of more oxygen than with natural oxytocin triggering contractions (described as like pushing them underwater then not lifting them out long enough to draw a breath before they’re back under again AKA fetal distress, or the lack of blood supply to the placenta caused by the epidural induced hypotension. The author has every right to raise these concerns as they are occurring thousands of times a day in the ‘developed’ world because people appear to only be concerned about epidural side effects for the woman and not the baby.
I’m a doula and a mother of 5. I had two hospital births with all the talked about negative side affects. I then had 2 unmedicated water births. What a different experience. Natural is better, period. (My 5th is due in 3 months and I have had to literally firght the medical community to have a birth the way I want because of the fear attached with water births and nonmedical interventions.) Our bodies were made for this. Animals do it without pain medication beucase they don’t have any other option.
I think it’s sad that because in America the epideral is so easy to get we feel entitled to it. When a women is in pain, she may not be thinking about the effects the epideral will have on her baby. She is only concerned with taking the pain away. This is why education beforehand is important. Not to mention support by doulas and midwives who truely have the mother and baby’s best interest at heart. In other countries, a lot of time due to lack of money, an epidural isn’t even an option. Mother’s expect it will hurt and deal with it just fine. The infant mortality rate and many other startling statistics are just now showing us how much better these other countries are doing compared to us. Check out the infant mortality rate of Norway and other European countries. In the 1960’s we (US) were rated 12th in 2004 we’re now rated 29th in the world! In case you missed it that’s death of the baby!(http://www.cdc.gov/nchs/ppt/nchs2010/44_MacDorman.pdf)
I believe that the people who have had a medicated birth and then an unmedicated birth really understand the differences. Someone that has had an unmedicated birth and then chose an epideral comment and tell me that the medicated was better, under the “normal” birth circumstances. I usually hear so many people that are advocates of epiderals arguing for the epideral when that is all they’ve ever known. I don’t think I’d have much credibility about my opinion on what it’s like to be blind if I have my sight, just because it’s my opinion or because I read what it was like.
These statistics that most are ignoring are scientific and proven. Here’s another article below stating the effects of the epideral. Those of us with experience see it time and again, the less you interfere with birth the better. Once you introduce just one procdure, usually many more must follow, it’s a snowball affect. So obviously epiderals and medical interventions have their place, at the right time and under the right circumstances. What this article and others are trying to say is that you can’t argue with the statistics that are just now being uncovered. Educate yourself, birth is painful, it’s also temporary pain. These statistics and experience with negative outcomes are forever. I bet hind sight being 20/20, those that had a bad experience wish they could go back and just have the pain of labor versus a baby that now suffers forever because of bad decisions made during the painful moment.
——————————————————————–
Epidurals–Real Risks for Mother and Baby
Epidurals–Real Risks for Mother and Baby (excerpted)
by Sarah Buckley, Brisbane, Australia
An epidural will often slow a woman’s labour, and she is three times more
likely to be given an oxytocin drip to speed things up (Ramin et al.,
Howell). The second stage of labour is particularly slowed, leading to a
three times increased chance of forceps (Thorpe et al.). Women having their
first baby are particularly affected; choosing an epidural can reduce their
chance of a normal delivery to less than 50% (Paterson et al.).
This slowing of labour is at least partly related to the effect of the
epidural on a woman’s pelvic floor muscles. These muscles guide the baby’s
head so that it enters the birth canal in the best position. When these
muscles are not working, dystocia, or poor progress, may result, leading to
the need for high forceps to turn the baby, or a caesarean section. Having
an epidural doubles a woman’s chance of having a caesarean section for
dystocia (Thorp, Meyer et al.)
When forceps are used, or if there is a concern that the second stage is
too long, a woman may be given an episiotomy, where the perineum, or
tissues between the vaginal entrance and anus, are cut to enlarge the
outlet and hurry the birth. Stitches are needed and it may be painful to
sit until the episiotomy has healed, in 2 to 4 weeks.
As well as numbing the uterus, an epidural will numb the bladder, and a
woman may not be able to pass urine, in which case she will be
catheterised. This involves a tube being passed up the urethra to drain the
bladder, which can feel uncomfortable or embarrassing.
Other side effects of epidurals vary a little depending on the particular
drugs used. Pruritis, or generalized itching of the skin, is common when
opiate drugs are given. It may be more or less intense and affects at least
25% of the women who take them (Lirzin et al. & Caldwell et al.): morphine
or diamorphine are most likely to cause this. Morphine also brings on oral
herpes in 15% of women (John Paull).
All opiate drugs can cause nausea and vomiting, although this is less
likely with an epidural (around 30% [ibid]) than when these drugs are given
into the muscle or bloodstream, where larger doses are needed. Up to a
third of women with an epidural will experience shivering (Buggy et al.),
which is related to effects on the bodies heat-regulating system.
When an epidural has been in place for more than 5 hours, a woman’s body
temperature may begin to rise (Camman et al.). This will lead to an
increase in both her own and her baby’s heart rate, which is detectable on
the CTG monitor. Fetal tachycardia (fast heart rate) can be a sign of
distress, and the elevated temperature can also be a sign of infection such
as chorioamnionitis, which affects the uterus and baby. This can lead to
such interventions as caesarean section for possible distress or infection,
or, at the least, investigations of the baby after birth such as blood and
spinal fluid samples, and several days of separation, observation, and
possibly antibiotics, until the results are available (Kennell et al.).
****There is a noticeable lack of research and information about the effects of
epidurals on babies.****** Drugs used in epidurals can reach levels at least as
high as those in the mother (Fernando et al.), and because of the baby’s
immature liver, these drugs take a long time–sometimes days–to be cleared
from the baby’s body (Caldwell, Wakile et al.). Although findings are not
consistent, possible problems, such as rapid breathing in the first few
hours (Bratteby et al.) and vulnerability to low blood sugar (Swantstrom et
al.) suggest that these drugs have measurable effects on the newborn baby.
As well as these effects, babies can suffer from the interventions
associated with epidural use; for example babies born by caesarean section
have a higher risk of breathing difficulties (Enkin et al.). When
monitoring of the heart rate by CTG is difficult, babies may have a small
electrode screwed into their scalp, which may not only be unpleasant, but
occasionally can lead to infection.
There are also suggestions that babies born after epidurals may have
difficulties with breastfeeding (Smith, Walker) which may be a drug effect
or may relate to more subtle changes. Studies suggest that epidurals
interfere with the release of oxytocin (Goodfellow et al.) which, as well
as causing the let-down effect in breastfeeding, encourages bonding between
a mother and her young (Insel et al.).
(An edited version of this paper was first published in Australia’s Parents
magazine, Aug/Sept 1998)
References:
-Buggy D, Gardiner J. The space blanket and shivering during extradural
analgesia in labour. Acta-Anaesthesiol-Scand 1995; 39(4): 551-553
-Caldwell LE, Rosen MA, Shnider SM. Subarachnoid morphine and fentanyl for
labor analgesia. Efficacy and adverse effects. Reg Anesth 1994;19:2-8
-Caldwell J, Wakile LA, Notarianni LJ et al. Maternal and neonatal
disposition of pethidine in child birth–a study using quantitative gas
chromatography-mass spectrometry. Lif Sci 1978;22:589-96
-Camman WR, Hortvet LA, Hughes N, et al. Maternal temperature regulation
during extradural analgesia for labour. Br J Anaesth 1991;67:565-568.
-Enkin M, Keirse M, Renfrew M, Neilson J. A Guide to Effective Care in
Pregnancy and Childbirth. P 287 Oxford University Press 1995
-Goodfellow CF, Hull MGR, Swaab DF et al. Oxytocin deficiency at delivery
with epidural analgesia. Br J Obstet Gynaecol 1983; 90:214-219
-Howell CJ. Epidural vs non-epidural analgesia in labour. [Revised 6 May
1994] In: Keirse MJNG, Renfrew MJ, Neilson JP, Crowther C. (eds)
Pregnancy and Childbirth Module. In: The Cochrane Pregnancy and Childbirth
Database. (database on disc and CD-ROM ) The Cochrane Collaboration; Issue
2, Oxford: Update Software 1995 (Available from BMJ publishing group,
London)
-Insel TR, Shapiro LE. Oxytocin receptors and maternal behavior. In
Oxytocin in Maternal Sexual and Social Behaviors. Annals of the New York
Academy of Sciences, 1992 Vol 652. Ed CA Pedersen, JD Caldwell, GF
Jirikowski and TR Insel pp 122-141 New York, New York Academy of Science
-Kennell J, Klaus M, McGrath S, et al. Continuous emotional support during
labor in a US hospital. JAMA 1991;265:2197-220
-Lirzin JD, Jacquintot P, Dailland P, et al. Controlled trial of
extradural bupivicaine with fentanyl, morphine or placebo for pain relief
in labour. Br J Anaesth 1989; 62: 641-644
-Paterson CM, Saunders NSG, Wadsworth J. The characteristics of the second
stage of labour in 25069 singleton deliveries in the North West Thames
Health Region. 1988. Br J Obstet Gynaecol 1992;99:377-380
-John Paull, Faculty of Anaesthetists, Melbourne. Quoted in: “The perfect
epidural for labour is proving elusive” New Zealand Doctor. 21 Oct 1991
-Ramin SM, Gambling DR, Lucas MJ et al. Randomized trial of epidural versus
intravenous analgesia during labor. Obstet Gynecol 1995; 86(5):783-789
-Swanstrom S, Bratteby LE. Metabolic effects of obstetric regional
analgesia and of asphyxia in the newborn infant during the first two hours
after birth I. Arterial blood glucose concentrations. Acta Paediatr Scand
1981; 70:791-800
-Thorp JA, Meyer BA, Cohen GR et al. Eppidural analgesia in labor an
cesarean section for dystocia. Obstet Gynecol Surv 1994; 49(5): 362-369
Reprinted from Midwifery Today E-News (Vol 2 Issue 7 February 18, 2000)
To subscribe to the E-News write: enews@midwiferytoday.com
For all other matters contact Midwifery Today:
PO Box 2672-940, Eugene OR 97402
541-344-7438, midwifery@aol.com, Midwifery Today
So just to be clear, as you kind of allude to but gloss over coming right out and saying it…. Did you or did you not have an epidural when you gave birth? Your ability to self justify and rationalize is impressive.
What do you mean “self-justify and rationalize”? I’m curious as to your thoughts on that. But yes, I had to have an epidural my first.
Hey Tracy, there’s a bit of a fallacy in the following: “If there were no reason for pain in childbirth, there wouldn’t be any, so obviously it’s there for a reason.” Not quite true. Pain doesn’t have to be selected for: One can reasonably argue that it’s an inevitable by-product of the considerable trauma the body has to go through to get a large-headed fetus to pass through a very narrow passage (plus necessary preparations, i.e. contractions, etc.). Because people don’t die of pain, the only reason why pain would be selected against is if it caused enough distress to mess up the labour process and therefore cause the death of the mother and/or baby (or harm either of their future reproductive outcomes). I have no medical knowledge on the topic, but one could say that the fact that mothers’ bodies produces endorphins at all is a sign that, to a certain extent, some natural protection against pain has been selected for – maybe just enough so that the pain itself doesn’t prevent labour from occurring normally in the vast majority of mothers. Sadly, evolution hasn’t come up with the miracle of making the whole thing entirely pain-free.
OK, back to my own work. 🙂
Hey Patricia! I do believe that pain is a natural by-product of the process of birth. However, at the very least it seems that the fact we do have endorphins tells us that the pain is necessary to a degree, but we are protected against it (to a certain degree). It may just be that it is there to ensure women know they’re in labour and can get to a safe space (thus protecting the life of mom and baby – an evolutionary purpose), I would believe, though, that there may be more to it. However, I fully acknowledge that it may be there as a by-product and simply not “selected out” so to speak – good catch (and thank you) 🙂
How is your work going?
I have never had an epidural, but I did have a shot of pethidine: http://www.babycentre.co.uk/pregnancy/labourandbirth/painrelief/pethidine/
Be sure to scroll down to the list of disadvantages: “It crosses the placenta and may affect your baby’s breathing and make her drowsy for several days, particularly if your birth progresses more quickly than expected and your baby is born within two hours of the drug being given to you.”
My baby was affected by the drug and her breathing stopped several times during the first week or so of her life. Thankfully, she didn’t need resuscitation and we were able to buy a baby monitor that bleeped when her breathing stopped.
I will NEVER use any drugs in labour again, aside from gas & air (maybe). No one clearly explained the dangers to my unborn child before I got that shot.
I hadn’t heard of pethidine – I don’t know if it’s offered here, but that’s crazy! How terrifying for that first week – I don’t blame you at all for not wanting anything again. I’m just so glad your daughter was okay in the end.
Tracy,
Pethidine is what we call in the U.S., Demerol.
Thank you 🙂
Interesting article… I had an epidural with my first and had an incredible experience of childbirth with no ill side effects and a perfect baby who latched on immediately…. If I decide I need one for my next child (due in 6months) I will not hesitate to have another….information on this topic is important, respecting what IS a personal decision (one between a mother/father/doctor, etc who all have the the best of intentions) is equally important.
I am 22 years old and went into my labor planning to be drug free for many of the reasons noted in this article. A day into labor and I was unable to stay conscious. I was dialated 7cm and so close to the birth that I wanted but I was unable to do anything but vomit and pass out. I decided at that point (as much as a semi-conscious person can decide) to have an epidural. Within 10 minutes I was able to be back in the room. After another hour, it was time to push. I pushed for 10 mintues when the doctor came in and said I wasn’t progressing and she wanted to do a c-section. Shockingly, it was 15 after 5. My child’s father politely informed the doctor that I was not going to have a c-section and that she needed to stay in the room and actually be helpful. Not 5 minutes later I gave birth to a healthy baby boy. And right after that, a nurse tripped over my IV line, ripping it from my arm. Altogether, the experience was nothing like I wanted it to be. I must say though, were it not for the epidural, I probably would have been forced to have a c-section because I was unable to stay conscious long enough to push.
I know this article is going to be difficult for a lot of women to read, because understandably so, we have a tendency to get quite defensive about our birth experiences. Unfortunately, like just about every aspect of birth, epidurals are not an isolated issue. For example, if a woman chooses not to have an epidural, she also needs to have a good birthing support system. If you’re going to go natural, hiring a doula is helpful, knowing good natural pain relief techniques is imperative, good positioning is a must, etc.
Most importantly, you can’t convince women about the benefits of turning down an epidural when they don’t have faith and trust in their bodies. Women today are very, very scared of birth, and for good reason….we have made it into a horror show and women don’t want to “put themselves through all that”. The only remedy for this is to encourage all our pregnant friends to take a GOOD prenatal course, like BirthWorks or Hypnobirthing….a course that helps women explore their own beliefs about birth and builds their confidence to not only give birth, but make decisions that aren’t based in fear!
Worth a read…
[…] childbirth. I had chosen to pursue a medication-free childbirth with my son 3 years ago for several reasons, the least of which may have been a fear of needles. My friend was also interested in pursuing it, […]
I find blogs like this to be psychologically harmful to women. Since when did women use the words regret and “my” when it came to giving birth? How can one “own” an experience? Having a baby is one of the most uncontrollable experiences that one may have. To tell a woman that it is something to own and that she should regret it if it doesn’t go the way she would like is ridiculous. It seems like those who have had a “natural” birth love to brag about it on the internet as if they have done something special. The only thing I regret about my birth experience is reading blogs that tell me I should regret it. Thanks….
Who on earth said you should regret anything?
I am definitely one of those women that regret everything about my birth experience. I had taken private hypnobirthing courses with a hypnotherapist for 5 months leading up to my due date. I did my visualization practices with my hubby every day and my own practice listening to the hypno cd every night. I had a vision board and talked positively about birth to anyone that would listen. I was excited, prepared, and so motivated to have my natural birth. I was absolutely looking forward to the challenge and ignored everyone that told me I was foolish to think “deep breathing” would get me through. 9 days past my due date, and no sign of baby, I was forced into an induction. 2 days into the induction with it going absolutely nowhere (4 doses of hormone gels, waters artificially ruptured, pitocin drip) I gave up my hopes of the hypnobirthing working and went for the epi. My contractions were SO intense and completely irregular, sometimes getting a handful in a few minutes with no break in between. It was so obvious my body was doing nothing naturally, and even though my baby wasn’t showing any signs of distress, nothing was happening. Finally, I was told a vaginal birth just wasn’t going to happen since my girl wasn’t even engaged, was in the stargazer position and hadn’t moved 1 iota down the birth canal. They knew this the entire time, but still tried to force her out that way, and gave me hope that my natural birth would happen, even though I truly believe it was always going to end up being a caesarean because she was not coming out on her own. I must say, being wheeled into surgery was the scariest experience of my life and I will never, ever forget the feeling of such intense fear. It was my worst nightmare. In a way, I resent the hypnobirthing, because it told me that whatever I envisioned for my birth experience would come true and that staying positive would equal success and thinking or even learning about negative birth experiences might cause my own to go in a similar direction. I was so unprepared for the opposite of what I wanted to actually occur. This was 14 weeks ago and I still get this sick feeling in the pit of my stomach when I think about what I went through, especially when I hear other friends who did not prepare in the way I did talk about their successful natural labours. On the bright side, all the drugs seemed to not have an affect on my BFing and my daughter and I have a very successful relationship there.
I’m so sorry that was your experience. I’ve never done hypnobirthing, but I do hate when people say it’s all in your head. Sometimes it’s not and you shouldn’t be made to feel as though *you* failed simply because your birth was one of the few that truly wasn’t going to happen the way you planned. I am glad your breastfeeding relationship was good though – it’s always nice when something goes right, eh?
Every medical professional I encountered before and during my birth minimized the risks of the epidural. I was encouraged to have an induction four days after my due date, was pumped full of pitocin, and was actually encouraged to get the epidural. Now I am stuck with an incurable, extremely painful spinal disease called adhesive arachnoiditis, a nerve disease that involves symptoms similar to MS, all of which resulted from the epidural. It is clearly a dirty secret in the medical community, as women would never sign the consent form if it were on it, and epidurals are big money. I will likely never be able to have another child. So yes, there are VERY good reasons to go natural, and women NEED to be made aware of these reasons. Go to theaword.org to learn more.
I was lucky, I had two labors with no pain relief whatsoever, no paracetamol, no gas. However this seems increasingly unusual, and not only that but people who chose to have a ‘natural’ labour are starting to be seen as ‘hippies… Risking their child’s health for their own beliefs.’
While we are lucky to live in a country where pain relief is an option, and it absolutely should be there for those who need it, it should not be seen as necessary to get through labour. This does nothing to prepare women for the amazing process that is labour. Yes it hurts, but understanding that the pain is ‘good’ and not a sign that something is wrong really helped me get through things mentally. We should do more to educate women about the labour process rather than simply offering them a menu of pain relief.