By:
Sarah Ockwell-Smith
Wendy Middlemiss
John Hoffman
Kathleen Kendall-Tackett
Helen Stevens
Darcia Narvaez
James McKenna
Tracy Cassels
(for a full list of author credentials, please see the end of the piece)
“My baby is only happy in my arms, the minute I put her down she cries.”
“She wakes every hour throughout the night, every night, I’m exhausted.”
–Statements frequently spoken by new parents
Waking at night and expecting comfort from parents is something most infants do. The number of times infants wake and need help to return to sleep decreases as they grow but still remains fairly common. Recent research by Weinraub and her colleagues confirms how normal it is for babies to wake at night, with 66% of 6-month-olds still waking at least once or twice a week and the remaining babies waking even more often. Some babies will cry when waking at 12 months of age—even babies who have settled back to sleep on other nights.
Helping an infant return to sleep easily, then, is an essential gift to give our infants—as well as an important goal for parents who need to rest. The science of nighttime care provides a good foundation for parents trying to calm their babies. It clarifies what is important to know about calming babies and why certain types of calming are most likely to be helpful.
What is Important to Know about Calming
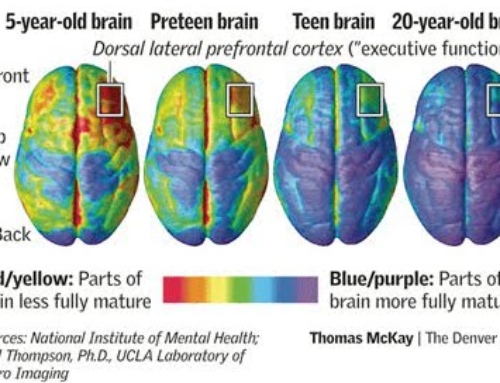
* A parent’s presence helps to calm babies who awaken in an upset state. Babies (especially in the first few months) are not yet capable of regulating their emotional states. This is one of the reasons why crying tends to increase in the first two to three months of live and then decrease steadily after that. Infants cry or fuss for many reasons, including hunger, pain or other discomforts or, at times, simply a desire for physical contact. For example, carrying infants from 3 to 4 hours a day reduces the duration of infant crying/fussing behavior generally by as much as 43% at six weeks of age (Hunziker & Barr, 1988).
Fussing and crying are the most important means by which an infant communicates needs and desires. The specific reason cannot always be determined, but for sure, display visible and audible signs of distress is an infant’s most important defence and is overwhelmingly adaptive. When upset, babies depend on sensory input from caregivers—touch, soothing voice, smell, eye gaze, breastfeeding—in order to calm down. That’s the way nature designed it to work. Babies rely on their caregivers to calm them and to help deal with other reasons they are unhappy or uncomfortable such as being in pain, hungry, or in some sort of physical or emotional state that we can’t determine. Being present and attending to infants when they wake and cry can help infants return to sleep more quickly (Mao, Burnham, Goodlin-Jones, Gaylor, & Anders, 2004).
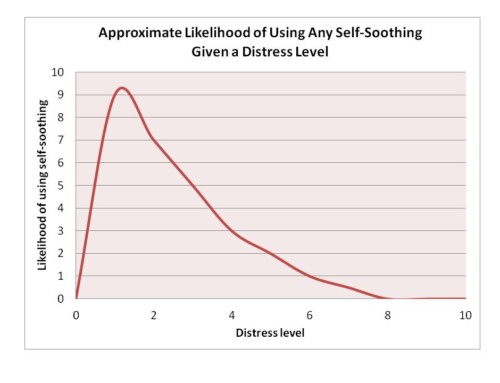
* Calming infants helps infants learn to calm themselves. By helping infants calm down by attending to their distress, caregivers help infants develop the tools—both physiologically and emotionally—to calm themselves. This is what parents help children with generally (Davidov & Grusec, 2006; Stifter & Spinrad, 2002). Parents are often hesitant to be present when babies cry, fearing that in attending to crying babies will lead babies to be unable to deal with distress on their own. But this approach only leads to a fussy baby and a clingy child. Leaving babies to cry increases babies’ stress levels and often keeps them awake longer. It does not guide them emotionally or physically toward the goal of regulating their own distress and response. Instead, to develop “good” or “healthy” sleep habits, gentle parental guidance is needed to resettle. Over time this leads to a strong, self-settling child who can calm him or herself when challenges arise.
* Understanding why some babies fuss more at night than other babies. Fussing upon awakening is a perfect normal behaviour. When babies are distressed they are indicating a need for attention, often to help them recover a feeling of security. It is, however, important to understand that babies differ in what makes them feel secure. Because some infants don’t cry very much or very forcefully, some people develop the expectation that all babies can/should be like that. But babies vary greatly in terms of how often and how hard they cry. These differences are driven by many factors, including temperament, experience and physiological maturity. Thus, the need for external regulation (calming) continues in varying degrees for different babies. Providing external regulation for babies who feel less secure and thus more distressed, actually helps them, not hinders them. It helps them build the neural pathways that eventually enable them to deal with stress and calm themselves (Cassidy, 1994; Stifter & Spinrad, 2002).
* Understanding when waking is a problem. Waking is a normal part of infant sleep and varies based on several infant factors: (a) feeding method (breast or bottle), (b) age, (c) shifts in developmental levels, and (d) individual level of maturity. In light of these factors, every family must determine whether an infants’ waking is a problem for the family. Waking isn’t a problem just because it happens. To suggest waking defines “problematic sleep” does not accurately reflect current science. We know that it is normal for infants to wake several times in the night, especially if breastfeeding. And given that human babies are neurologically immature at birth, awakenings are the infants’ major line of defence against dangerous, prolonged breathing pauses and permits oxygenation. Moreover, transient and more prolonged awakenings can help respond to cardio-pulmonary challenges while asleep and restore a more natural heart rhythmicity (Mosko et al 1997a). Recall that the early research on sudden infant death syndrome (SIDS) revealed that infants who woke frequently in the night were less likely to die of SIDS than those who awakened significantly less often (see review in McKenna 1995 and Mosko et al 1997a and b).
After babies are beyond the age of chief risk for SIDS and their waking and sleeping is settling into more of a consistent pattern, research shows that many continue to wake in the night (Weinraub et al., 2012). Even then it may be more helpful to frame the night waking as a family problem rather than as a child’s “sleep problem.” If a parent is OK with a baby waking two or more times a night at 12 months then there is no problem!
Bottom line: Crying upon awakening is a perfect normal behaviour. Helping crying infants feel comforted and calm supports their developing abilities to calm themselves over time.
Calming Ways to Calm Babies
The first three months of life is known to many as ‘The Fourth Trimester’ and requires similar care to the womb. Some babies make the womb to world transition easily, others less so. Many of the ways parents naturally try to calm babies actually re-create many of the comforting, familiar experiences infants had during their time in utero. For all babies, these calming techniques can be very comforting.
* Recreate movement. The womb is a constantly moving space and babies tend to respond by calming to movements such as dancing, swaying from side to side, going for an exaggerated quick walk or bumpy car ride.
* Rely on touch; provide skin to skin contact. Being in contact with warm, naturally (un)scented, skin is proved to be calming for infants/babies, it helps to stabilise their body temperature, heart rate and stress hormones and stimulates the release of oxytocin – the love and bonding hormone – in parent and baby both.
* Recreate familiar sounds. The babies’ time in the womb was marked by many rhythmic sounds. Sounds similar to those babies heard in the womb can be very calming. White noise offers constant surrounding sounds while also slowing brain wave frequencies.
* Help the infant learn to deal with sensations of hunger. Hunger is a new sensation for infants—and infants may find it hard to calm when they feel hungry. Feeding babies when they wake at night can help babies transition back to sleep, especially when lighting and interaction are kept at low levels of stimulation. Babies also find sucking to be the ultimate relaxation and comfort tool, one of their few forms of self initiated self-regulation. Sucking helps a baby’s skull bones to return to their normal position after birth as well as providing them with comfort and security. Some infants/babies respond to sucking on a dummy/pacifier as soothing (but avoid this in the early weeks of breastfeeding as it can pose problems establishing breastfeeding). Non-nutritive suckling on the breast is also calming.
Sleep Routines that Can Help Calm Babies
Parents can help recreate these calming environments across any sleep routine and sleep pattern. What is important to remember is what is calming and why. Some sleep approaches that may help include these below.
* Keep babies close. Keeping babies close helps in shared breathing, touch, warmth, and awareness of any difficulties. Babies are generally much calmer and sleep more easily if they are sleeping with their caregivers or in very close proximity. Babies can benefit from the shared breathing (and general sensory exchanges) with the caregiver including skin to skin contact and this can achieved to varying degrees depending on the overall safety conditions including keeping the infant on a separate surface next to your bed, a behaviour called separate-surface cosleeping. Many breastfeeding mothers find that intermittent bedsharing helps them with their breastfeeding, especially if they work during the day. Bedsharing (while recommended against by the American Academy of Pediatrics) not only increases sleep time both for mothers and babies but has the effect of increasing the chances that mothers will breastfeed for a greater number of months than if they place their infant elsewhere for sleep. But close proximity usually means night feeds are much easier, there are more of them, and they are far less disruptive for parents and infants and thus can be more settling. That said, just as with any sleep arrangement, bedsharing does carry risks (as does sleeping away from the baby) and there are very clear circumstances that we know that make bedsharing not advisable.
When bedsharing should be avoided. It is important for the caregivers to refrain from bedsharing if they are not breastfeeding, and obviously if any adult is under the influence of alcohol or drugs or anything than may impair their natural arousal patterns. Surely, babies should sleep alongside the bed on a different surface (a) if adult bedsharers are excessively sleepy, (b) if smaller children are likely to find their way in to the parents’ bed, or (c) if there is another adult present in bed who refuses to take any responsibility for the infant. Bedsharing should be avoided if mothers smoked during pregnancy because infant arousal patterns may not be as efficient as they should be for maximum safety in a bedsharing environment. The same holds true for small premature infants. They are safest sleeping alongside the bed in a different sleep structure rather than in the bed. And, finally, it is highly risky to fall asleep with an infant on a couch, sofa or armchair as many infants have suffocated by being trapped between the adult and some part of the furniture. In all these cases, co-sleeping (different surface, same room) is more advisable than bedsharing.
Finally, wherever an infant sleeps they should always be placed on their backs. Moreover, if sleeping with or away from caregivers, infants should be positioned away from soft bedding, pillows, or toys and be situated so that breathing is never unobstructed with their heads never covered.
You can download a pamphlet on safe co-sleeping here (and below in the references).
* Breastfeeding. In addition to all its other associated benefits to infant health and cognitive development, breastfeeding is an excellent way to calm a baby. It provides skin-to-skin contact and warmth. Breastfeeding can be of benefit to the caregiver as well, making wakings easier to manage and helping to reduce postnatal depression (Fergerson, Jamieson, & Lindsay, 2002). Further, mothers who are exclusively breastfeeding actually get more sleep and are less tired during the day than mothers who either exclusively use formula or both breast- and formula-feed (Kendall-Tackett, Cong, & Hale, 2011).
* Listen to the baby & trust your caring instincts. Babies are master communicators, just as adults typically are masters at figuring out how best to respond. Adults don’t learn to rock a baby or to talk softly…these come naturally. So to calm babies, it is helpful to follow the baby’s lead and follow one’s heart. Parents need to learn to follow their hearts and keep babies safe and healthy. If holding the baby seems to cause distress, then parents can stay with them, but place them in a position that seems more helpful. If the parent is still, perhaps walk; if the parent is already moving, perhaps rock. Parents should trust their instincts in how to be present with the baby.
Note to Parents: There is only one expert in your baby – you. Sometimes you will find a way to calm your baby easily; sometimes it may seem like what worked before doesn’t work now. But, being patient with your baby and with youself will help you both learn and grow.
What if the Routine is Still Stressful?
A time may come when a parent start thinking, “I’ve been doing night-time comforting for quite awhile now. . . Is there anything I can do to move towards getting some uninterrupted nights?”
The answer is yes. Partly it comes with time – varying times for different babies as Weinraub’s recent study showed. And there are some things parents can do to gently move in that direction with the baby. We will later share some ways to help babies need less attention at night, if that is something that is essential for a family’s well-being. These approaches will build on the essential steps for calming discussed here:
- Listen to the baby’s signals
- Provide nurturance and support
- Help babies help themselves calm.
To download this post as a Press Release, please click here.
Bibliography/References*
Cassidy, J. (1994). Emotion regulation: Influences of attachment relationships. Monographs of the Society for Research in Child Development, 59, 228-283.
Davidov, M. & Grusec, J.E. (2006). Untangling the links of parental responsiveness to distress and warmth to child outcomes. Child Development, 77, 44-58.
Fergerson, S.S., Jamieson, D.J., & Lindsay, M. (2002). Diagnosing postpartum depression: can we do better? American Journal of Obstetrics and Gynecology, 186, 899-902.
Hunziker, U.A., & Barr, R.G. (1986). Increased carrying reduces infant crying: A randomized controlled trial. Pediatrics, 77, 641-648. ftp://urstm.com/CharestJ/Articles.pdf/Hunziker%20U%201986.pdf
Kendall-Tackett, K.A., Cong, Z., & Hale, T.W. (2011). The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. Clinical Lactation, 2(2), 22-26.
Mao, A., Burnham, M.M., Goodlin-Jones, B.L., Gaylor, E.E., & Anders T.F. (2004). A comparison of the sleep-wake patterns of cosleeping and solitary-sleeping infants. Child Psychiatry and Human Development, 35, 95-105.
McKenna, J.J. (1995). The Potential Benefits of Infant-Parent Co-Sleeping in Relation to SIDS Prevention, by In Torliey O. Rognum, Ed., SIDS in the 90s. Scandinavian Press, 1995.
McKenna, J.J., & Mosko, S. (1990). Evolution and the Sudden Infant Death Syndrome (SIDS) Part II: Why Human Infants? Human Nature 1 (2).
McKenna, J.J., & Mosko, S. (1990). Evolution and the Sudden Infant Death Syndrome (SIDS), Part III: Parent-Infant Co-sleeping and Infant Arousal, Human Nature: 1(2).
McKenna, J.J., & Mosko, S. (2001). Mother-Infant Cosleeping: Toward a New Scientific Beginning, in R. Byard and H. Krous, eds., Sudden Infant Death Syndrome: Puzzles, Problems and Possibilities. London: Arnold Publishers.
Mosko, S., Richard, C., & McKenna, J. (1997). Infant Arousals During Mother-Infant Bed Sharing: Implications for Infant Sleep and SIDS Research, Pediatrics 100 (2): 841-849.
Mosko, S., Richard, C., & McKenna, J. (1997). Maternal Sleep and Arousals During Bedsharing with Infants, Sleep 201(2): 142-150.
Stifter, C.A. & Spinrad, T.L. (2002). The effect of excessive crying on the development of emotion regulation. Infancy, 3, 133-152.
Weinraub, M., Bender, R.H., Friedman, S.L., Susman, E.J., Knoke, B., Bradley, R., Houts, R., Williams, J. (2012). Patterns of developmental change in infants’ nighttime sleep awakenings from 6 through 36 months of age. Developmental Psychology, 48, 1501-1528.
*NOTE: Many of the references are available for downloading at: www.cosleeping.nd.edu, where there are extensive details and conversation pertaining to the safety and controversy of bedsharing, covered both by an interview at the website and the FAQ section of the website.
Co-Authors
Sarah Ockwell-Smith, babycalming.com
Wendy Middlemiss, University of North Texas
John Hoffman, uncommonjohn.wordpress.com
Kathleen Kendall-Tackett, Texas Tech University, www.uppitysciencechick.com/sleep.html
Helen Stevens, Safe Sleep Space
Darcia Narvaez, University of Notre Dame, www.psychologytoday.com/blog/moral-landscapes
James McKenna, Mother-Baby Behavioral Sleep Laboratory, University of Notre Dame, www.cosleeping.nd.edu
Tracy Cassels, University of British Columbia, www.evolutionaryparenting.com



In the first paragraph- it says that 66% of 6 month olds still wake in the night once or twice a WEEK- do you mean a night? Also there are quite a few typos. But great article!
Molly Schaffer
Hi Molly,
Nope – the findings were per WEEK not night.
Tracy
Regarding the instruction to always put babies to sleep on their back: Pelligra, Doman, Leisman (2014) http://www.iahp.org/reassessment-sids-back-sleep-campaign-12232014/
Hi, in this very helpful article you mention “We will later share some ways to help babies need less attention at night, if that is something that is essential for a family’s well-being”…where can I find this? Sorry if it’s very obvious! Thanks
This was part of a series and I don’t know that that part made it up! It’s a hard topic and one that often doesn’t work well from a mass advice perspective as each baby and need is different. How old is your baby?