It seems a week can’t go by without another article going viral by someone trying to dismantle the “benefits of breastfeeding” (or really the risk associated with formula use, as the biological norm is breastfeeding). One could almost think that this justification for formula use is being peddled by the formula companies themselves, but alas, it seems to be women fighting to see their use of formula as equal to breastfeeding. The biggest issues in the research according to these many articles?
- That the effects for breastfeeding, when present, are small and thus overstated; and
- That there is that nasty confound with socio-economic status (SES) in that higher SES women are more likely to breastfeed, less likely to face various diseases, and have higher IQ.
You can read about these in almost any mainstream article that attempts to justify the way in which formula is now the socially “normal” way to feed a child. I’m not going to say these problems aren’t real – they are – but rather that they also ignore one of the bigger problems in breastfeeding research. What is this research problem? Put quite simply, it’s the way in which groups are formed when we’re making comparisons about breastfeeding outcomes.
I’m not surprised no one talks about this because it’s actually a problem in that it results in the underestimation of the effect of breastfeeding. That’s right: This problem actually means that our “small” results may really be much larger and some null results may be type II error (i.e. failing to detect an actual difference where one is present) in that we have erroneously failed to reject the null hypothesis because our groups are made in such a way as to bias our results towards a failure to find any significant differences.
How Grouping Works
When you design a study where you want to compare various groups, you have to have pretty strict rules for who belongs in which group. This is great in terms of trying to make claims if your groups are well-defined and theoretically distinct, but with something like breastfeeding, it’s nearly impossible to get the kinds of groups you want. For example, the most common type of comparisons are any breastfeeding for a certain duration versus no breastfeeding or less than for a certain duration, like any breastfeeding at 3 months versus no breastfeeding at 3 months.
Why would this be problematic, you ask? First you have to think about how much breastfeeding is going on. Is it exclusive? Is it 70% of the time? In these groups you will have the mom that exclusively breastfed for 2 ½ months but stopped when going back to work because pumping didn’t work in the non-breastfeeding group and the mom who breastfed no more than 20% of the time and stopped altogether at 4 months in the breastfeeding group, yet which one do you think would have a bigger impact on their child’s health? This gets to be even more complicated the longer the duration is (e.g., when analyses are done at six months).
When you get into exclusive breastfeeding, which should be simpler on the surface, you also run into problems as you now have the mom who struggled and may have given only one bottle (or only for one week while working with a lactation consultant) no longer eligible for the exclusive breastfeeding group despite the fact that her child is going to be far more like the exclusive breastfeeding child than the child who has formula 90% of the time. Or what of the child who has solids introduced at 5 months? Is the effect assumed to be the same as that of the child who has been receiving 50% formula all along? (Hint: nope.)
The complications here stem from the fact that breastfeeding is not an all-or-nothing act and the shades of gray are very difficult to properly categorize yet likely have important implications for the outcomes of interest. In all these categorizations, however, the bias still leads us away from finding the benefits of breastfeeding/risks of formula because the only “pure” group would be those who followed WHO guidelines and exclusively breastfed on demand for 6 months then continued to nurse for approximately 2 years or more (some children wean before that and they would be biologically normal). That is the biological norm for which humans have evolved (or were created, depending on your perspective) and the effects of breastfeeding need to be examined through that lens.
Any criticisms of small effects in groups that includes less than this for a breastfeeding group – especially groups that include mixed feeding early – presupposes that the effects of breastfeeding are huge (akin to some kind of panacea) or that there is no interaction with formula use or amount of breastfeeding. Yet that’s not what those who study breastfeeding or its impact on health are arguing. In fact, it seems to be brought up as such only by those looking to dismantle breastfeeding research because their job is much easier if you hold breastfeeding up to such a high standard that it simply has to fall apart (or if it stands up to such scrutiny, there’s no sense in saying formula is any kind of equal). The researchers themselves are simply limited by the data they have, yet others seem to assume this is some kind of intentional grouping based on the magnificent power of breast milk.
How should groups be made then? When people talk about the ideal grouping methods, the randomized control trial is considered ideal yet it’s impossible in breastfeeding research. In this, you randomly assign who will fit into each condition. In drug trials, it’s ideal: One group gets the drug, another a placebo (or another drug), and you compare outcomes. In breastfeeding we not only can’t dictate who will or will not breastfeed, but we can’t dictate how someone breastfeeds or for how long and we certainly can’t keep people blind to the status of the women and children in the study. Thus we are left with the incredibly messy task of trying to put people with such diverse situations into well-defined groups, a task that makes our interpretation of results very problematic.
The Previous Research
As mentioned, all of the previous studies suffer from this grouping problem. Whether it’s the randomized control trial (of breastfeeding promotion, not actual breastfeeding) in Belarus (also known as PROBIT)
Despite all of the grouping problems, however, there is a trend in the research that is worthy of consideration: The closer we get to the biological norm for breastfeeding, the more significant the results become. That is, when looking at specific diseases or intelligence or educational attainment or whatever else is theoretically linked to breastfeeding, when exclusive and enduring breastfeeding are included, we almost inevitably see significance in some key areas (luckily no one assumes breastfeeding influences everything).
Using cancer as an example, the research on breastfeeding and childhood cancer is often considered to be mixed, yet the more one looks into the research in detail, patterns emerge that are to do with (a) specific subtypes of cancers, and (b) the length and exclusivity of breastfeeding. In some cases, it’s not until that norm is reached that we can see the risks of formula use. (For a full examination of the breastfeeding-cancer link, read here.) The recent Brazilian research also highlighted this with the effects becoming stronger with a longer duration of breastfeeding and more “predominant” breastfeeding.
What Does This Mean?
Most importantly, going forward we need more studies that actually examine outcomes in groups that include enduring, exclusive breastfeeding, 50% mixed feeding, and 100% formula use to help us understand the effects of both mixed feeding and full formula use. After which we can start to examine the nuances between these groups to determine if there are certain points at which risks start to kick in, for nuances there are, and it’s important for us to understand this.
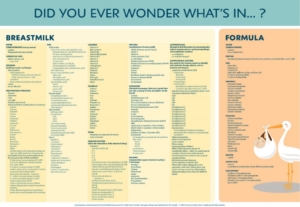
I realize there is a huge push to argue that “even one breastfeed counts” or the like, but the problem is that this feeds into the notion that breastfeeding is some magical elixir when in fact, it may not be. Our bodies have evolved (or were created) for a type of biologically normal breastfeeding which includes approximately six months of exclusive breastfeeding on demand followed by breastfeeding complementing other foods for years after. Although a look at the ingredient list between breast milk and formula definitely highlights the real difference between the two, it’s really unclear how much breastfeeding is necessary to meet our biological norm. Or rather, how much formula changes our biological norm. Notably, this research shouldn’t be undertaken to shame anyone, but to help us better understand how our moving away from what is evolutionary or biologically normal influences our health in the short- and long-term.
Equally importantly, we need everyone to understand that the effects of breastfeeding (or not) are dynamic, not static. They will differ based on one’s personal experiences, genetic make-up, environment, and so on. Understanding these nuances is central to getting a better idea of how to help families and children. In addition to the grouping problem, we also have the problem that breastfeeding is assumed to influence each individual the same way yet that’s likely not true. For example, a child exposed to various environmental toxins or various diseases is likely going to benefit more from the influence of breastfeeding than a child in a healthier environment to begin with. In one case, it may be the difference between life and death, the other, only small differences.
With respect to how we’ve interpreted the data as a whole thus far, it is clear that the studies we have are far from perfect. It also means that all these studies that purportedly have found no differences are very conservative estimates of any effect of breastfeeding/risk of formula and people should be aware of this, especially if people are going to bring up the SES issue. You see, when people bring up the SES issue, they should also be willing to admit that although that may bias results liberally, a far greater concern is with the groupings which has a much greater chance of biasing results conservatively.
Why is this concern greater? Because SES variables are being included and controlled for, therefore the main concern remains with causality and residual confounding. That is, we still cannot say the effects are definitely causal, only correlational, and there may be other effects of SES that we haven’t controlled for that would influence the findings. Now, we have some studies that actually do demonstrate potential causality (see here for an example), but we cannot control for residual confounding and thus it remains problematic. However there is no control for the grouping problem. Once someone is in a group, they are there for better or worse, and when our groups are so loosely defined, trying to extrapolate the data to others becomes incredibly difficult. Frankly, given this, I’m always amazed when any research finds any effects of breastfeeding.
The real question, however, and one we need to consider moving forward, is whether we can even examine the real effects of breastfeeding in a society where biologically normal breastfeeding is so rare. Not only is there a huge social push away from this type of breastfeeding, but even finding women who are exclusively breastfeeding at six months is difficult as our cultural norms are so very far from our biological norms.
Breastfeeding research is flawed, though not only in the way that most formula apologists would like you to believe. If we are ever going to truly understand the amazing nature of breast milk and breastfeeding, we need to start looking at it from its evolutionary basis as not only food, but something more that has helped us thrive and survive against what would seemingly be all odds.
***
If you are in need of individualized parenting help, I offer services via email, Skype, and phone on a variety of parenting topics. You can find out more here.
_________________________________
[1] Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, et al. Promotion of breastfeeding intervention trial (PROBIT). JAMA 2001; 285: 413-20. [2] Colen CG, Ramey DM. Is breast truly best? Estimating the effects of breastfeeding on long-term child health and well-being in the United States using sibling comparisons. Social Science & Medicine 2014; 109: 55-65. [3] Victora CG, Horta BL, de Mola CL, Quevedo L, Pinheiro RT, et al. Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. The Lancet Global Health 2015; 3: e199-e205.






Finally!!!! I have been touching on this issue for YEARS. I became very frustrated many years ago participating in an online survey, because the child in question had started “solids” at 5 1/2 months. He was barely having any and was exclusively breastfed otherwise, but he didn’t get to count as exclusively breastfed because he’d had a couple of bit of mashed banana.
I have 4 kids and only 2 of them have been completely, exclusively breastfed for 6 months. Of the other 2, 1 had a bottle of formula in the hospital when my milk took 5 days to come in, nursed exclusively until 5 1/2 months and started tiny amounts of solids at that point, gradually increasing as he got older. He had another bottle of formula when he went on a 15 days nursing strike at 10 months old. The formula pushed him back to nursing (although only to sleep, sadly) and he continued to nurse until he was nearly 3. The other one nursed exclusively until about 5 1/2 months when he literally screamed for our food. I had hoped to wait until at least 6 months, but as he was long past all the milestones for being ready and was losing his mind whenever we ate, I started giving him real food. He’s still nursing at 4o months old.
They would both undoubtedly be grouped with kids who had been having formula for months before that 6 month point.
Yea! Awesome to see this. I have had this problem when trying to participate in questionnaires in the past. My 1st was a NICU baby and had expressed breastmilk and formula for the first month, then had 1 bottle of formula a day until he weaned (due to pregnancy and a bad sinus infection) at 14 months…then he started nursing again at 20 months and continued to nurse several times a day until 3 1/2. Obviously he was a ‘mixed-feeding’ baby, but did he ‘wean’ at 14 months? Or 42 months? And surely his 1 bottle of formula is a lot different than 50% mixed feeding? Then I was really sick with bronchitis at the birth of my 2nd babe and my body was so depleted from being sick, dehydrated, and labor itself my milk didn’t come in at first. I gave *one* bottle at 3 days, then she was exclusively breast feed until 6 months when she started solids and continued to nurse until around 26 months. But I can’t say she was ‘exclusively’ breastfed because she had that one bottle out of 26 months. I get that she was not exclusively breastfed, she had outside food in her developing digestive track at only 3 days old, but to count her as in the same statistics on how breastfeeding does or does not affect humans babies as the baby who only breastfed for the 3 days when mom was in the hospital and then switched to formal is not sound science.
What is it that you’re hoping to gain from better research, though?
At this point, I think most people know that there are real benefits to breastfeeding. If they choose not to, then, it’s not because they don’t care about those benefits, but because of other, individual factors. Those factors are varied, personal, and valid, and it should be utterly out of line for anyone to criticize.
I am all for working toward public policy that makes it easier for those who want to breastfeed to do so. But the moment this steps toward haranguing those who choose otherwise, you lose me.
Better information of course! A lot of people discount the benefits to breastfeeding. If you think they are accepted, you need to read about the many people out there claiming there are none and the many people believing it!
I also wonder if whether the mother was breastfeed as a baby or not also has an effect.
[…] Une réflexion intéressante sur les problèmes rencontrés quand on fait de la recherche autour de […]
You say that researchers have difficulty finding children who were breastfed for 2 years, including 6 months exclusive. My kids fit the description. Is there a way to contact researchers who need subjects for their research? Perhaps there should be some kind of bank of people to contact when you need subjects who have been breastfed for 2 years/6 months EBF.
It’s a wonderful idea. I would recommend looking at your nearest university to see if any researcher is studying breastfeeding and get in touch with their lab!
Thank you for this. We who have been studying the effects of breastfeeding for a long time have been thwarted by the lack of sound research based on a sample of mothers that have been divided into the appropriate groupings. I see some of the comments here and am not sure if the article has cleared up the confusion. In research on breastfeeding we need to have clear criteria on who belongs in each group. The group that is practicing the biological norm and has done from the beginning and the group that has deviated for whatever reason. This means that if the baby has received any other food for example except breast milk that they cannot be said to be exclusively breastfed for the purposes of research. It is not a judgment it is a necessary part of research to keep it specific enough to mean something. Historically the two groups have been muddy and not indicating the true effects for breastfeeding exclusively. Actually having a bank of mothers who would fall into the first category might be good and from this group a way of randomizing who participates in the study. Someone should make a web site to submit possible participants in the study.
Just seen this. A really good overview on why BF research is problematic. I’d add one further major difficulty – outcome measures that are not crystal clear, that have inbuilt social or personal biases, or which no one can agree how to measure anyway I’d put all IQ/cognitive/behavioural outcomes in that category. We can fairly happily count hospital admissions (quigley et al with uk millennium cohort data), gastro episodes (Dundee cohort), medical diagnoses (of diabetes, for example). But outcomes such as problem-solving ability (assessed by parents), intelligence (er……what is intelligence?!), and a whole ton of other subjective, socially and culturally specific messy stuff…..? I don’t think so.
Great reading. Another aspect is the child who has had only breastmilk, but given in a bottle alot of the time…changes alot also. I have exclusively breastfed all four of my children. None had food before 6 months. And all continued on the breast until at least 2years, one until almost 5. I have never been approached to be part of any studies. It would be great if this type of clear statistical information reporting were conducted with vaccinated vs non-vaccinated health.
‘Biologically normal’ does not mean EBF to exactly 6 months. It means till the baby shows signs of wanting food. Better to group as ‘approx 6 months’ and ‘at least 95% breast milk’.
Absolutely!! Though really from an evolutionary perspective, foods between 5-6 months, some as young as 4 months, but not before then.
This was brilliant.