There are two new research articles out that complement each other quite nicely and highlight a very critical issue when it comes to parenting: The relationship between breastfeeding and infant sleep. Although many “experts” like to ignore that sleep patterns will differ in crucial ways (and not others) when a child is exclusively breastfed, the fact is that feeding method can have a profound impact on not only how our child sleeps, but how us parents interpret their sleep.
The first study of note is a qualitative, exploratory study from Dr. Helen Ball’s Lab at Durham University
When discussing sleep with these families, mothers who were currently using formula strongly believed the societal view that formula feeding and sleep go hand-in-hand, that formula feeding is associated with better or more sleep (despite research showing this isn’t actually the case[2][3]). Breastfeeding mothers, on the other hand, didn’t really buy into that train of thought, but reported facing a lot of pressure to switch to formula when their infant’s sleep didn’t match the societal ideal of 8 hours a night, even when babe was very young (4 weeks, as reported by one mother).
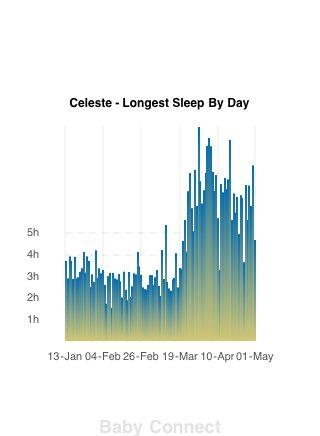
Another distinction came in the view of sleep strategies. Namely, formula-feeding mothers argued that a routine/schedule is key in order to return to pre-baby life (or as one mother put it, “I believe that a baby fits round your routine, you don’t fit around theirs”) whereas breastfeeding mothers were more likely to discuss the overhaul to one’s life or a change in lifestyle and the need to work around the needs of the baby. In line with these views, it should be no surprise that formula-feeding mothers were far more likely to report using extinction sleep training (cry-it-out and controlled crying) methods early and often whereas breastfeeding mothers reported using close proximity for sleep (bedsharing or room-sharing). Very interestingly, the mothers who previously formula-fed and now breastfeed and use shared-sleep space as the new model report that it is superior for their own sleep than their previous arrangements of sleep training and using formula. Of note, this mom isn’t the only one, here’s a graph from a mom who measured the sleep she got pre-bedsharing and post-bedsharing and she was breastfeeding so there were no bottles to make up or anything:
Perhaps none of this is surprising to many people. Although I have seen my fair share of unbelievably responsive and cue-based parenting in formula-feeding moms, there is enough evidence highlighting the generalized dichotomy in sleep parenting and feeding method that was highlighted herein. The question becomes, do all families feel this way? How do we identify which behaviours are associated with problematic sleep? Is co-sleeping and breastfeeding really creating “bad habits” that will hurt our kids later on?
Enter the second study of note, from researchers in Ireland[4]. The goal of this study was to examine the differences between families based on infant sleep patterns and maternal health, providing insight into whether or not there really are sleep differences in infants (or sleep behaviours in the family) that result in poorer maternal health (likely due to sleep deprivation). As this study was population-based, the sample is large with over 11,000 families participating. Due to the sheer size of the sample, the study was questionnaire-based, with families reporting on infant sleep at 9 months, parental stress, maternal health and depression, smoking, alcohol use, infant feeding (i.e., ever breastfeed and currently breastfeeding), as well as demographic information. Using this data, the researchers conducted what’s known as a cluster analysis. This is a method that uses the data entered to create groups of people that are similar in certain ways and significantly different from the other groups based on the same data. In the current analysis, four distinct groups were identified.
Before we talk about the groups, it’s worth noting here that at 9 months of age, only 16% of infants were reported as not waking at night, meaning 84% of babies were regularly waking at night, adding further support to the notion that night waking is incredibly common and biologically normal in this age group. A sizeable minority (12%) reported that baby’s sleep was a moderate-large problem.
Now, what of the groupings? The first two groups (of four) were quite similar except for one difference: group 1 had infants that did not wake at night whereas group 2 was made up of infants who did wake. However, they were otherwise identical: Similar total sleep durations for babies and mothers, babies slept in their own cot, and no mothers reported infant sleep as a problem. The second two groups differed from the first two in terms of infant and maternal sleep duration (both lower on average, but within the normal range). In group 4, all infants were sleeping in their own cot whereas in group 3, 85% were sleeping in the parental bed, 11% with siblings, and only 4% in their own cot. Thus, group 3 may be seen as the “co-sleeping” group. There were also differences in the groups in terms of perceived sleep problems, with all families in group 4 reporting that their infant’s sleep problems were at least a small problem and over 34% reported them as moderate-large problems. In group 3, nearly half said sleep was not a problem, 27% said it was a small problem, and 25% said it was a moderate-large problem.
Already we can see that bedsharing itself does not seem to cause problems, nor do night wakings per se. After all, nearly 50% of the sample is in group 2 who reported regular night wakings and no sleep problems and the 13% of the sample that was in group 3 (the “co-sleeping” group) who were getting less sleep were also less likely to report sleep problems than the solitary sleep group (group 4). The question now is how these clusters relate to maternal health.
Due to the large sample sizes, every value was statistically significant, but luckily the authors included a measure of practical significance. When looking at practical significance, there were three small associations and one moderate association, though none of the comparisons included demographic confounds such as ethnicity, income, or education which are all related to maternal well-being.
There was a very small association with depression scores, with the mothers in groups 3 and 4 having a higher rate of scores above the cut-off. What is unknown is if these correspond to the mothers in the group reporting a large problem or not. There is also a small association with alcohol use, with mothers in group 3 (the “co-sleeping” group) most likely to abstain and mothers in the other three groups being comparable in terms of use (quite moderate all around). The final small association is to do with ever breastfeeding, with mothers in group 1 (no night wakings) being least likely to have ever breastfed, mothers in groups 2 and 4 being more likely, and mothers in group 3 (the co-sleeping group) being most likely to have ever breastfed. This fits with the one moderate association which is current breastfeeding. Infants in both groups 3 and 4 were more likely to be currently breastfeeding, with the highest rate in group 3.
How do we understand these studies together?
The first issue seems to be the relationship between infant sleep and breastfeeding. Whereas the Rudzik and Ball[1] paper found there to be emerging qualitative evidence that formula-feeding is associated with viewpoints about what “good” sleep is, this was somewhat confirmed quantitatively in the Hughes and colleagues[3] paper. Those who were least-likely to breastfeed or be breastfeeding were most likely to have a baby who slept more at night perpetuating the idea that breastfeeding itself causes sleep disruption or that formula is a fix for sleep. However, the quantitative study by Hughes and colleagues also shows us the flaws in this logic. There were families who were not breastfeeding and who had infants who woke at night, only they didn’t seem to view this as a problem at all, and parents who were breastfeeding and had infants who didn’t wake or woke and it posed no problems. Thus, there seems to be something in the parents that leads to this view. The very small relationship between the groups and depression may highlight that it isn’t sleep that causes the depression, but rather the depression that causes sleep disruption, in line with other findings (for a review, see [5]).
The second issue is dealing with the common adage that you are instilling “bad habits” in your child by doing things like nursing to sleep or bedsharing or responding to night wakings. As Rudzik and Ball discuss, this is actually very common for breastfeeding mothers and helps them with respect to their own sleep and baby’s sleep. In the Hughes and colleagues paper, although there were individuals in the co-sleeping group who reported problems, there was an entire group of people who weren’t co-sleeping who reported problems as well, thus suggesting another etiology for the problems. However, the data from Hughes and colleagues dismisses the idea of “bad sleep habits”, specifically nursing to sleep and night wakings, as night wakings were found in the vast majority of groups, including those who weren’t breastfeeding (thus not nursing to sleep) or co-sleeping. Parents should rest assured that this builds upon other long-term data[6][7] that shows how biologically normal these acts are.
The final area worth discussing, as both papers do, is the idea that sleep problems are most often driven by views of the parent. Both papers mention in their discussion that infants are displaying biologically normal behaviours (even in the “less sleep” groups for the Hughes and colleagues paper, the infants were getting a normal range of sleep), but some parents seem to view them as problems whereas others don’t. This is in line with previous research conducted in the United States[8] that found parental reports of normal infant behaviours being deemed “problematic” was linked to things like higher parenting stress, more stressful life events (outside parenting), and low socio-economic status. What Rudzik and Ball add to this is that it may also be in part due to or contribute to feeding choices (the direction is unknown). Are parents who are more likely to buy into the notion that children should be sleeping through at an early age more likely to choose formula because it fits with their conceptions of how to raise their children? Much more research is needed on why some parents feel this way and others don’t, but I do believe this is the crux of the issue that we need to know in order to help families.
What’s the take-home message here? Primarily that we simply cannot treat feeding and sleep as separate issues when it comes to our babies. The relationship between the two is huge and decisions on one front will intimately affect the other. At a time when 40% of moms aren’t meeting their breastfeeding goals[9], one area that we should look into is that of how we discuss and treat their infant’s sleep. Perhaps if we can help families understand what is biologically normal, we can help them feed how they want and sleep more. That seems a laudable goal to me.
To read up on safe bedsharing, please check out the EP pamphlet on the issue here.
***
If you are in need of individualized parenting help, I offer services via email, Skype, and phone on a variety of parenting topics. You can find out more here.
_______________________________
[1] Rudzik AEF, Ball HL. Exploring maternal perceptions of infant sleep and feeding method among mothers in the United Kingdom: a qualitative focus group study. Matern Child Health J 2015; DOI: 10.1007/s10995-015-1798-7 [2] Kendall-Tackett K, Cong Z, Hale TW. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. Clinical Lactation 2011; 2: 22-6. [3] Doan T, Gardiner A, Gay CL, Lee KA. Breast-feeding increases sleep duration of new parents. J Perinat Neonat Nurs 2007; 21: 200-6. [4] Hughes A, Gallagher S, Hannigan A. A cluster analysis of reported sleeping patterns of 9-month old infants and the association with maternal health: results from a population based cohort study. Matern Child Health J 2015; DOI: 10.1007/s10995-015-1701-6 [5] Douglas PS, Hill PS. Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review. J Dev Behav Pediatr 2013; 34: 497-507. [6] Hysing M, Harvey AG, Torgerson L, Ystrom E, Reichborn-Kjennerud T, Sivertsen B. Trajectories and predictors of nocturnal awakenings and sleep duration in infants. Journal of Developmental and Behavioral Pediatrics 2014; 35: 309-16. [7] Weinraub M, Bender RH, Friedman SL, Susman EJ, Knoke B, Bradley R, Houts R, Williams J. Patterns of developmental change in infants’ nighttime sleep awakenings from 6 through 36 months of age. Developmental Psychology 2012; 48: 1511-1528. [8] Goldberg WA, Lucas-Thompson RG, Germo GR, Keller MA, Davis EP, Sandman CA. Eye of the beholder? Maternal mental health and the quality of infant sleep. Social Science & Medicine 2013; 79: 101-108. [9] Perrine CG, Scanlon KS, Li R, Odom E, Grummer-Strawn LM. Baby-friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics 2012; 130: 54-60.





Great article! Breastfeeding was not going well for me early on. Co-sleeping saved our nursing relationship. Nursing drowsily helped us both relax and boosted my milk supply. Wish more Americans could dialogue about this topic without the judgment.
Great article- thanks for sharing. Our Liam is 10 months old and I know for a fact he isn’t getting enough sleep at night, waking 3-5 times and we bed-share. I am debating trying to move him into his own sleeping space but still in our room. He is formula fed and not really eating anything else like food wise. I am not going to do a CIO method but instead look at gentle transitions. If it doesn’t work I am going to just go back to bed sharing as it does work even though he wakes up.
Good luck! One thing to note is that 3-5 wakings is on the upper end, but not actually abnormal in that age group. The 9-15 month age range is FILLED with transitions that disrupt sleep. I would look for cues of sleep deprivation instead of hours in bed.
What I’m really curious about is the long term effects on babies who are formula fed on schedule and put in a crib vs babies who are breastfed and cosleep. What difference does it make when that baby is grown up? I was formula fed myself as a baby and I’m a happy healthy independent adult and my mother loves me. I’m now raising a baby of my own and I breastfeed. I’ve recently started to cosleep for my babies sake as he gets more rest this way during teething and separation anxiety. So ultimately, what consequnce is faced??
A huge piece is the individual temperament of the child as to what long-term outcomes can be seen. Not all babies do well bedsharing. We also know there are tangible risks to feeding on a schedule so even though you came out just dandy, you came out dandy *despite* being fed on a schedule, not because of it. For some children, scheduled feeding has led to hospitalization and death 🙁 Following your child’s cues is going to be best in all cases 🙂
There are many babies who have been formula fed and are well adjusted adults and there are certainly plenty of breastfed babies who are intolerable adults. I would be inclined to believe that you can nurture and love a baby very deeply either way and that loving your baby and doing your best for them must be the most important thing you can give your child.
As well, it’s certainly possible to formula feed on demand.
One other item of note is that some babies have died while breastfeeding as well. I’m just curious how adults are ultimately affected in the long term. It seems a very tricky thing to track with studies.
Andrea, when we talk about statistics and research we are talking about risks. Yes, there are many healthy adjusted children on formula because formula feeding is just one factor while parenting is thousands of factors. Just because there are many healthy children on formula doesn’t mean that breastmilk is not more beneficial -it is. Also just because there are some children on breastmilk with poor health doesn’t mean they would be the same or better on formula – they would be worse.
And as you said it’s totally possible to formula feed on demand. It is also position to schedule breastfeed. While breastfeeding makes it easier to be responsive to the baby, it is not determinant .
[…] Understanding the Important Relationship Between Sleep and Feeding Method | Evolutionary Parenting |…. […]
[…] Evolutionary Parenting […]
[…] Ter ere van Wereld Borstvoeding Week een Zondags Leesvoer met enkel artikelen over borstvoeding. Alle afbeelding zijn uit de oorspronkelijke blogs. #WBW2015: Protecting ALL Women in ALL Types of Work ‹ Reader — WordPress.com. Global Health Media Project – New breastfeeding videos for mothers. Guest Post: Learning To Trust Our Children Through Sleep Struggles | Evolutionary Parenting | Where History And Science Meet Parenting. Understanding the Important Relationship Between Sleep and Feeding Method | Evolutionary Parenting |…. […]