A new study out of Pediatrics
First let’s start off by admitting that they did try to examine a pretty important question: What are the risk factors for death at different ages? This is important because most parents assume the risks remain the same when in fact, this may not be the case at all, and what is a safe sleeping environment at one age may not be safe at another. However, what they have actually answered is more akin to looking at the situations that infant deaths occur in when compared only to other infant deaths. In this regard, the authors found that younger infants (0-3 months) who died of SIDS or suffocation were more likely to be found in the parental bed than older infants (4-12 months) and were more likely to have been placed on their side or stomach (prone position). Older infants, on the other hand, were more likely to have other items in bed with them such as blankets, toys, stuffed animals, and more than younger infants.
What do we take from this? Well, not much. We have descriptive data for the environments infants are found in when they suffer SIDS or suffocation, but we have no data on how this compares to children who did not die, which is necessary to make any risk assessment. Although the authors claim that bedsharing is riskier for younger infants, it is equally likely that more infants bedshare in the 0-3 month age group because that is the time that they are often nursing throughout the night and bedsharing means that process becomes easier and parents sleep better. As infants start to sleep longer stretches, parents may be more likely to put their infants in a cot for those longer times.
If we look at the data, it seems a risk may not even be present. In this dataset, 73.8% of infants aged 0-3 months were bedsharing at time of death while only 58.9% of older infants were bedsharing at time of death. For this to be a higher risk, this has to be a higher percentage than naturally occurs in this age group as if the naturally occurring number is the same, then just by sheer chance, a similar proportion should be found (assuming no additional risk factors). Although this research does not speak to that, one study of nearly 300 mothers asked what their sleep practices were with their 3-month-old infants found that 72% admitted to bedsharing regularly[2]. (Note that other studies have found lower rates, but it’s unclear what the rate actually is. Many parents don’t admit to bedsharing but do practice it. Many parents say they do not bedshare because it’s not an intentional practice yet bring their baby to bed every night for a period. In short, we need more data that really addresses all types of bedsharing when talking to parents.)
If we use these numbers, the relative risk ratio would clearly be non-significant at 1:1.025, meaning that there would be a 2.5% increased risk for bedsharing without considering confidence intervals (and I can tell you from a lot of stats experience, that kind of increase isn’t going to result in significant differences above and beyond chance). Notably, if the numbers were to hold for the 4-12 month age group (which I don’t know), we could actually start to argue that not bedsharing becomes a risk (but somehow I doubt the numbers are the same given the same reasons mentioned above).
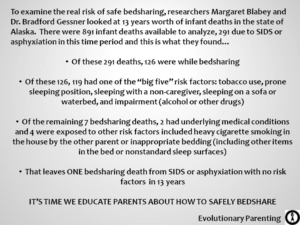
The other problem with this research is that by using nationally collected data, there is virtually no information on the main risk factors that interact with bedsharing. As reported elsewhere[3], when these risk factors (which include parental smoking, alcohol or drug use – including prescription and over-the-counter medications, soft mattress, too many blankets, prone sleeping position, non-breastfeeding, and more) are accounted for, bedsharing does not seem to indicate a higher risk for SIDS or suffocation. Another study[4] also found that the intentionality of bedsharing is critical to the issue of risk with intentional bedsharing not resulting in any increased risk of death whereas unintentional bedsharing is associated with an increase, likely due to the unsafe nature of unplanned bedsharing.
Does this new study tell us that bedsharing is “unsafe” or “riskier” for young infants? No. Not even close. All this tells us is that younger and older infants are dying in different environments when they die of SIDS or suffocation. This should not be too surprising as the environments for older and younger infants reflect the various needs and developmental stages they are at. As mentioned above, younger children tend to bedshare more than older ones given the ease of nursing and the ability to provide parents with more sleep. Unfortunately, not all parents actively seek to ensure a safe bedsharing environment, perhaps because education on the matter is so scarce in the face of anti-bedsharing campaigns.
Although the authors have attempted to speak of risk factors, the data they have examined simply cannot speak to that as there was no comparison with the actual prevalence rates of these behaviours in children that did not die. The authors attempt to paint their data as condemning of bedsharing, especially in infancy, and yet they have failed to not only accurately assess the risk of bedsharing, but have failed to capture any of the known risk factors that interact with bedsharing.
In short, this study adds nothing to question of how safe or unsafe bedsharing can be. All it does is continue to add to the dogma that bedsharing is dangerous whilst providing zero evidence to support that view and failing to consider the wealth of data that has been accumulated on the subject. So long as we continue to preach this dogma of unsafe bedsharing, we run the risk of setting new parents up to put their babies in unsafe sleep environments. As always, accurate and scientific education – not fear – needs to be the cornerstone of safe infant sleep advice.
Note: A more recent study did the appropriate analyses and found that the risk of SIDS for younger infants is NOT increased by bedsharing when other factors are considered.






Another example of decision-based evidence making rather than evidence-based decision making 🙁
Hey Meggie what do you mean by this?
[…] Does Bedsharing Increase the Risk of Death for Younger Infants? by Tracy Cassels BA, MA, at Evolutionary Parenting, discusses this article: Colvin JD, Collie-Ackers V, Schunn C, Moon RY. Sleep environment risks for younger and older infants. Pediatrics 2014; doi:10.1542/peds.2014-0401. […]
Hi Tracey – just wondering – have you ever engaged a SIDS educator/ representative and put your wealth of arguments to them to receive a response? If so, what was it?! Apart from a Cochrane Review on the issue, it would be great to see this actually nutted out head to head, rather than posted about/talked about here there and everywhere with all of it really just an ongoing, seemingly verbose discussion of contradictory advice to consumers (no offense intended, I’m hugely interested in the topic, I just would like a solid consensus!!) I a health worker in the public system and and would LOVE to see this debated within a group of respected ‘authorities’ on the matter (perhaps via live feed or on unedited youtube…)?
It depends on the educator. I am regularly in contact with other researchers like Helen Ball and James McKenna who look at this and agree with the main ideas behind what I’m writing, but would some of the others, like Carpenter? I don’t think so mainly because they seem to have their own agenda and search to make the data fit it. I am taking part in a conference in March on sleep where topics like this will be discussed (it’s an academic conference) and so we may see some head-to-heads there 🙂
But doing a debate would be great. I just don’t know who the best person would be.
Thank you for this. I hope that the incorrect guidelines, which are not so ‘NICE’, work for the good here by creating more articles like this one. It is hitting the mainstream media as well, seen here today in the Huffington Post – http://www.huffingtonpost.co.uk/zion-lights/parenting-advice_b_5597376.html so let’s be grateful for that, and keep sleeping safely with our babies.
[…] out this post for a more in depth look at what that much discussed study, showed and didn’t show. I also […]
What bugs me so much about all this is that suffocation deaths always seem to get lumped in with SIDS deaths. From what I know, there are risk factors that seem to increase the risk of SIDS, but ultimately there is no known cause. And the autopsy of the baby of a friend of mine who died of SIDS, had an inconclusive result- which to me, is what SIDS is all about, no? SIDS is sudden death- not death that can be determined to have another cause, like suffocation. Am I wrong? Other causes of death can be more prevented, like by not putting blankets or pillows or bumpers, etc., in the crib.
So why is suffocation death always relevant when talking about SIDS?
I would think that bedsharers are more likely to suffocate than other babies in empty cribs, so could they be included to boost the scary numbers?
I bedshare with my 3.5 month old and have since the start, but all the scary articles caused me to buy a Respisense at 6-7 weeks (because ALL bedsharing babies die between 6-10 weeks, right?).
Many times it’s because they can’t conclusively state suffocation or SIDS, but also I think doctors assume that it must be suffocation despite all the knowledge we have coming out about SIDS. But it’s true – it’s a problem in the way they lump the deaths together.
To be fair to the researchers, this study doesn’t seem to have been *meant* to look at the question of whether bedsharing increases SIDS risk or not. Rather, they’re looking at what part different *known* risk factors currently play in SIDS deaths that are still occuring.
As to your title question… well, we’ve now got four different studies looking at whether bedsharing increases the risk of death in younger infants (the Carpenter et al multicentre study in 2004, the McGarvey et al study in Ireland, the Venneman study you cited, and the Tappin et al study in Scotland) and all four of them found a bedsharing/SIDS association in younger infants, even after adjusting for things like smoking and bedding. That’s pretty good evidence that, yes, it does.
By the way, why did you think the Venneman study showed no increased SIDS risk with intentional bedsharing? Looks to me as though it shows the reverse: looking just at the group of usual bedsharers still showed an increased SIDS risk associated with bedsharing.
I had thought the same until I read THEIR comments about what they felt their research has shown.
Re the other studies – all have some rather serious flaws, including bad variables and missing known correlates to bedsharing (some include bedding but not all, measurement of alcohol use is flawed in some cases, etc.), which is why things like the Alaska study which actually examined all deaths due to SIDS and suffocation are essential to our understanding of any relationship. The Carpenter et al. multicentre study actually found that when mom didn’t smoke, bedsharing was NOT a significant predictor of SIDS (the CI crosses 1), but also their multivariate OR DOESN’T control for anything other than age and centre location which isn’t really a true multivariate that controls for these other variables. Only Table 3 which doesn’t examine bedsharing includes the variables in Table 2 for the multivariate factors.
The McGarvey study does control for more although there are concerns with some of their variables, like alcohol consumption which was defined as *any* alcohol consumption in the day prior which we know from other studies to often *underestimate* the effect of alcohol because it ignores the additive effect of quantity and the timing of alcohol, and selection, such as having the control cases be approximately 5 weeks OLDER than the controls. Even controlling for age, that doesn’t actually statistically help because the events would be different by age and that can’t be controlled for. Also, although they seem to imply they are controlling for tons of variables, in reality they are only controlling for smoking and social deprivation in the odds-ratio they provide. Their one multivariate OR that deals with usual patterns is something to look into, but as it involves age differences, problematic assessment of key variables, it’s difficult to make concrete suggestions (and more disturbing, the multivariate OR does NOT control for INFANT age although the univariate does, as it should). In short – it’s very difficult to take the study at face value.
Now, the Tappin et al study… Well, even their multivariate odds ratio was JUST significant; however, they only control for some variables. Notable amongst the absent variables controlled for are: tog value of bedding, alcohol or drug use, prematurity, and breastfeeding. In addition, when smoking is included only as “either parent” it underestimates the effect because the effect of dad (or other partner) smoking is far, far less than when mom who is next to babe smokes. This is why later studies have been clear to separate those two as it’s likely that the smoking variable herein is strongly underestimated. We also are not given the age at which the controls were interviewed which is critical (as mentioned above) for the “last sleep” interview.
As for the Venneman study – have you read the full report? The multivariate OR (which of course you want to look at over the univariate as that’s what’s controlling for the other variables) for parental bed as the “usual” place of sleep is 0.76 (non-significant relative to own bed, but still lower, and as the univariate is slightly higher but also non-significant, we either claim parental bed is as helpful to *preventing* SIDS when the usual place of sleep or that bedsharing does not increase the risk even at a univariate level).
Does this help?
Interesting thoughts. OK, there doesn’t seem to be a way to do them justice in the reply without running on at great length, so probably the best thing is if I split this comment to reply to your thoughts on each study separately, which I think (or at least hope) will make for marginally easier reading than a single humungously long comment. (I guess kh is getting her wish, anyway…)
The Carpenter 2004 study – I didn’t spot anything out of the ordinary about how the multivariate ORs were calculated, so I’ve gone back to it to check. Were you looking at the line at the bottom of Table 2 saying ‘ORs are adjusted for age and centres’? I suppose that *could* be read as saying that they were *only* adjusted for age and centres, but, apart from that being a such a bizarre way for anyone to analyse a study with this many variables that I can’t imagine the researchers doing it, it does explicitly state on the next page that ‘these ORs are adjusted for the effects of all the other factors in the model…’ which looks clearcut to me. So my interpretation of that line under Table 2 would be that it meant they included age and centres *as well as* the other variables. Or is there something else about this in the text that I’m missing?
The figure in Table 2 of that study for bedsharing does give a non-significant OR, but that’s the analysis with all ages lumped together. The results section says that the OR was progressively greater in younger infants, and the graph on page 187 showed it to be statistically significant in the youngest infants.
When you publish you HAVE to list in each table exactly what is controlled for therefore the ORs in Table 2 are ONLY controlling for age and centre.
The graph on p 187 shows that even at the youngest age it’s BARELY significant and given the lack of other variables included, it’s difficult to see this as supporting the idea of a risk for safe bedsharing.
McGarvey study – I’m puzzled as to why you say that they ‘seem to imply they are controlling for tons of variables’ they are only controlling for smoking and social deprivation? Table 1 specifies a long list of variables that the multivariate OR controlled for.
I agree that, theoretically, the lack of detail on *quantity* of alcohol use prior to sleep could have affected the results. In practice, though, I’m dubious you’d have that many families in which an infant death while bedsharing with alcohol-impaired parents would be diagnosed as SIDS, because the natural bias in those cases would be to diagnose it as some form of asphyxiation/overlying/neglect based on the history. In fact, if anything we’d probably get an underrepresentation of SIDS diagnoses for bedsharing infants of alcohol-impaired parents when compared to cot-sleeping infants of alcohol-impaired parents, for that very reason. But, of course, that’s speculation.
The difference in infant age – yes, fair point, that could be a factor if younger infants were more likely to be bedsharing than older ones, as that would skew the results.
Table 1. Look at the notation next to the bedsharing MORs by age then look at the bottom right corner of the notes. That’s how you know what those are controlling for and it’s ONLY smoking and social deprivation. The ones above it control for everything else.
Re alcohol, the problem with the assessment is for the CONTROL groups, not the SIDS groups. Or rather, how they interact. With this assessment, many people in the control group likely report some alcohol use (obviously likely less than that of the SIDS group), but the differences between thee two groups will be far less and therefore the OR becomes significantly undervalued. Make sense?
Infant age is also a problem in most control studies, but definitely a problem in this one.
Tappin study – multivariate OR for bedsharing under 11 weeks is hardly ‘just significant’. The lower border of the 95% CI was 2.99! I agree that not controlling for tog value of bedding is a problem with this study, and potentially the case/control age difference. Also possibly not controlling for alcohol intake, but, as the authors point out, that one’s been shown elsewhere not to interact with bedsharing when it comes to SIDS risk.
They did control for birth weight, which I think would be a reasonable proxy for prematurity (actually, possibly better than controlling for prematurity, since we don’t know whether the issue is respiratory immaturity or infant weight, so controlling for small-for-dates term infants may be important). Not controlling for breastfeeding would actually lead the study to *underestimate* bedsharing risk if anything, since you’d see higher rates of breastfeeding among the bedsharing group.
I don’t see why controlling for smoking as ‘either parent’ would be a problem? Dad smoking may be less of a risk than mum smoking, but since both are a risk, you’d need to control for both. I can’t see how controlling for them as a single variable would be any different from entering them as two separate variables, since what you want at the end of the day is the figure with both of those adjusted for. Am I missing something?
Look at Table IV – for non-smoking mothers, the lower end is 1.20 when infants are < 11 weeks. The alcohol issue is important as it HAS been found to be significant when assessed appropriately. The NZ cot study they cite had similar assessment problems as McGarvey. Anything is non-significant if you don't assess it well 🙂 Smoking assessment is a similar issue as I explained with alcohol. If you know mom is the big risk factor, it may be more moms smoke in the SIDS group whereas more dads smoke in the control group. Make sense? So you want to adjust for both separately. Breastfeeding can go either way. You THINK you'd see more breastfeeding in bedsharing, but possibly not with bedsharing DEATHS. Hence the need to control for it.
Venneman study – not sure where you’re getting the 0.76 OR from? I’m looking at the figures in Table 3, where they’re broken down not just by bedsharing during last sleep but whether bedsharing was usual or not. The group we’d want for this is the ‘bedsharing usual and bed shared during last sleep, which have a multivariate OR of 2.63, statistically significant, when compared to the reference group of non-bedsharers (non-usual bedsharers who also didn’t bedshare during last sleep). So that would mean bedsharing was still a risk even in the group who usually bedshared.
Bottom line: We’ve got consistent results across four different studies, which aren’t perfect but are of reasonably good quality overall in terms of assessing for confounders. That seems to me to be enough evidence to say, yes, there probably is a risk. (Also, of course, there’s the potential asphyxiation/wedging risk, which is also not zero and isn’t covered in the above studies, which only look at SIDS.)
By the way, I agree with you that we shouldn’t turn this into rigid anti-bedsharing advice, because that can backfire. However, as far as the question of risk goes, I think it’s fair to say that, yes, there almost certainly is a (slight) risk with bedsharing.
0.76 is from Table 2 – where the child has usually slept for the past 4 weeks and looks at parental bed. In Table 3, all of the sleep environments are included for bedsharing (parental bed, sofa, everything else) which may be skewing the results. However, even I have to admit that the results from Tables 2 and 3 don’t jive. From a statistical pov, it doesn’t make a lot of sense.
For me the bottom line is that these studies have big flaws – “reasonably good quality” is overstating it. They were great to highlight new variables assess in future research (which has happened) and we should look to them as starting points, which many have. But when you look at something like the Alaska study which looked at each and every death and found that they all had risk factors (except 1 in a multi-year period) and was looking at SIDS and asphyxiation, you start to see how the inherent flaws of the case control studies as they’ve been done are failing to grasp the importances of risk factors to death.
Btw, thank you for separating these – much easier! Sorry if I’ve seemed short in my replies but my computer is being weird and mouse is going everywhere making it REALLY hard to type!
Thank you, by the way, this has highlighted the need for an article on the flaws in these studies and how we need to move forward with the research 🙂
[…] Does Bedsharing Increase the Risk of Death for Younger Infants? by Tracy Cassels BA, MA, at Evolutionary Parenting, discusses this article: Colvin JD, Collie-Ackers V, Schunn C, Moon RY. Sleep environment risks for younger and older infants. Pediatrics 2014; doi:10.1542/peds.2014-0401. […]
[…] Does Bedsharing Increase the Risk of Death for Younger Infants? by Tracy Cassels BA, MA, at Evolutionary Parenting, discusses this article: Colvin JD, Collie-Ackers V, Schunn C, Moon RY. Sleep environment risks for younger and older infants. Pediatrics 2014; doi:10.1542/peds.2014-0401. […]
[…] Comentários da Dra. Tracy Cassels: link. […]
[…] • https://gku.flm.mybluehost.me/evolutionaryparenting.com/does-bedsharing-increase-the-risk-of-death-for-younger-infants/ […]
So I work for CPS and have seen my fair share of infant deaths. We also are required to explain safe sleep to all parents which includes warnings agains cosleeping. When my baby was born, I obviously had to nurse him throughout the night and was absolutely terrified to do it in bed bc of my experience. But, when I did it felt natural and I was able to control blankets and pillows so they were not near him. Instinctively knowing that mothers must have slept with their babies throughout history I started doing research and did not realize such contradicting info was out there. I realized that of all the deaths of babies I had seen none of them were due to suffocation by a sober parent, mostly being placed face down on an adult bed or becoming tangled in blankets or wedged in the wall. I’m lucky for my experience because I know now how to make cosleeping safe and have since been slowly feeling less guilt for cosleeping part of the night. I still have him sleep in his bassinet bc I do want him to learn independent sleep but the moments I have coslept with him have been magical and some of my best memories of parenting so far.
[…] • https://gku.flm.mybluehost.me/evolutionaryparenting.com/does-bedsharing-increase-the-risk-of-death-for-younger-infants/ […]
[…] https://gku.flm.mybluehost.me/evolutionaryparenting.com/does-bedsharing-increase-the-risk-of-death-for-younger-infants/ […]